Introduction
Mechanism of action
Indications
Common side effects
Serious side effects
Long-term side effects
GI tract damage
Cardiovascular effects
Renal toxicity
High risk populations
Reerences
Further reading
Introduction
Ibuprofen is a non-steroidal anti-inflammatory drug (NSAID) and is often used to reduce pain, tenderness, stiffness, and inflammation. In addition to treating these acute symptoms, ibuprofen can also be used in the management of various inflammatory diseases such as rheumatoid arthritis.
Despite the effective anti-inflammatory, analgesic, and antipyretic effects of ibuprofen, it is associated with numerous adverse effects that can cause significant damage to cardiovascular, renal, hepatic, and gastrointestinal (GI) tissues.
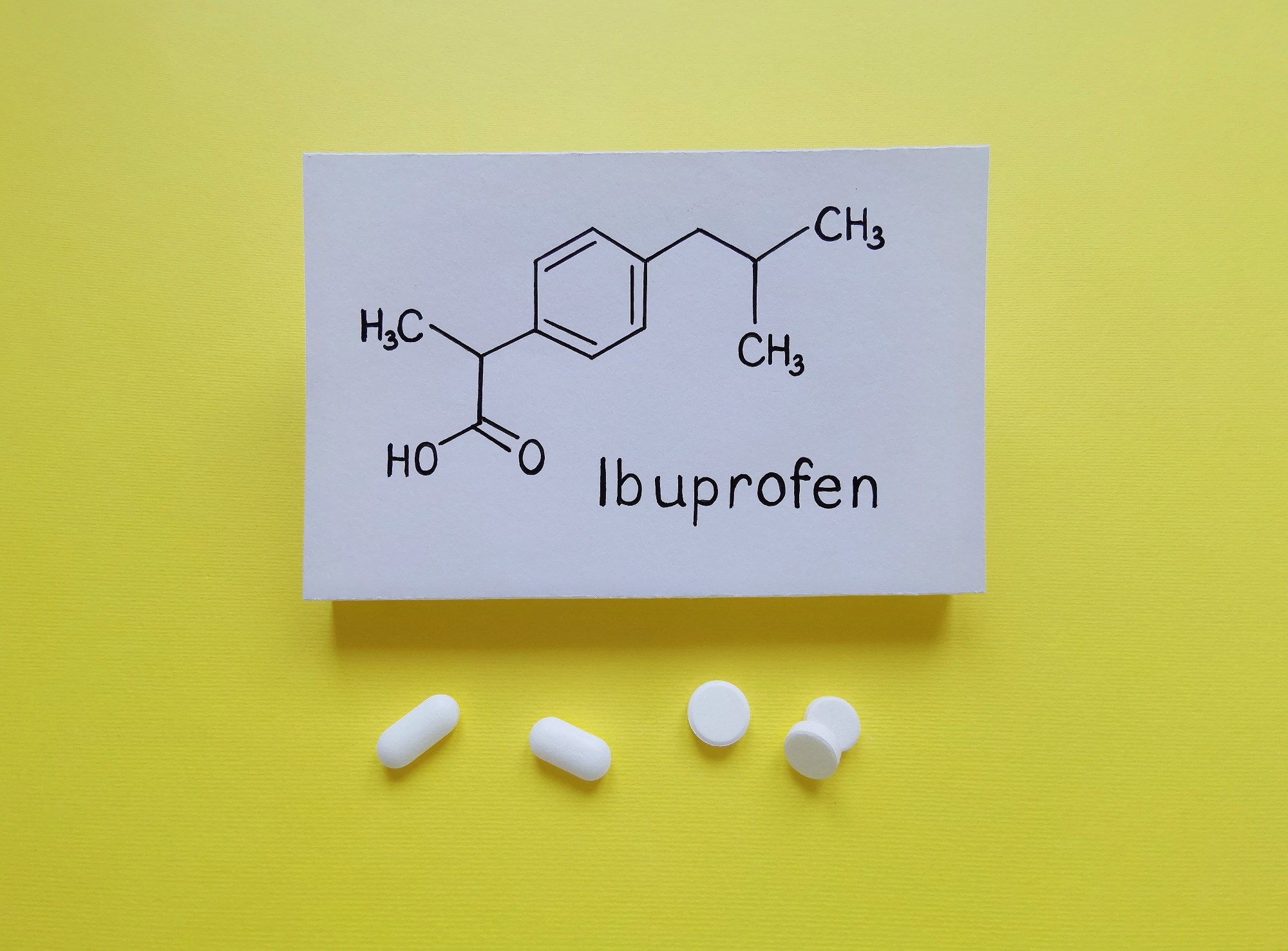 Ibuprofen is a medication in the nonsteroidal anti-inflammatory drug (NSAID) class that is used for treating pain and fever. Image Credit: Danijela Maksimovic / Shutterstock
Ibuprofen is a medication in the nonsteroidal anti-inflammatory drug (NSAID) class that is used for treating pain and fever. Image Credit: Danijela Maksimovic / Shutterstock
Mechanism of action
Ibuprofen is a non-selective inhibitor of cyclooxygenase 1 (COX-1) and (COX-2), both of which are isoforms of the COX enzyme. COX-1 is expressed in most tissues and is important in maintaining homeostasis, protecting the gastric mucosa, platelet aggregation, and regulating circulation within the kidneys.
Conversely, COX-2, expressed in fewer tissues than COX-1, is induced by the activity of various proinflammatory cytokines. Notably, the inhibition of COX-1 by ibuprofen is 2.5 times more potent than that of COX-2.
COX catalyzes the synthesis of prostaglandins from arachidonic acid. Thus, the inhibition of this enzyme reduces the expression of various prostaglandin precursor molecules that are implicated in inflammation.
Indications
In most countries, ibuprofen is available as an over-the-counter (OTC) drug in the form of oral tablets, lipid-based soft capsules, suspensions, chewable tablets, and topical gels. Ibuprofen can also be administered intravenously in a clinical setting.
When used to treat general pain in adults, the recommended oral dosage of ibuprofen is 200 to 400 mg every four to six hours as needed. At this dose, ibuprofen can treat mild-to-moderate pain from headaches, sore muscles, dysmenorrhea, achy joints, and fever.
Conversely, when used to treat arthritis, ibuprofen can be prescribed at a total dose ranging from 1,200 to 3,200 mg per day in three or four doses.
Common side effects
When taken orally, ibuprofen usage is associated with several minor side effects. These include:
- Headaches
- Dizziness
- Nausea
- Vomiting
- Gas/bloating
- Indigestion
These side effects are less commonly reported when ibuprofen is applied topically. However, these side effects may still occur, particularly when the topical solution is applied to a larger area of the skin.
Ibuprofen can sometimes cause the skin to become more sensitive to sunlight when used in gel, mousse, and spray forms.
Serious side effects
Although rare, several severe side effects may occur following ibuprofen usage. In the event that a patient experiences these side effects, they should immediately contact a doctor and/or go to the emergency room.
- Melina (black stool)
- Swollen ankles
- Blood in the urine
- Severe chest or stomach pain
- Chest tightness
- Difficulty breathing/wheezing
- Worsened asthma symptoms
- Severe headache
- High temperature
- Stiff neck
- Light sensitivity
- Blurred vision
- Hallucinations
- Itchy, red, swollen, blistered and/or peeling skin
- Swelling in the mouth, face, lips, tongue, and/or throat
Long-term side effects
NSAIDs are over-the-counter medications that are considered to be the most widely used drugs in the world. However, despite the efficacy of NSAIDs like ibuprofen in treating pain and inflammation, their usage, particularly at higher doses and for more extended periods of time, is associated with several toxic side effects.
GI tract damage
One of the most common adverse effects of ibuprofen usage is GI bleeding, which can lead to gastritis, ulceration, hemorrhage, or intestinal perforation.
The inhibition of COX1 is believed to be the primary mechanism by which ibuprofen causes GI damage, as this reduces the mucosal levels of prostaglandins, which subsequently causes damage to both the stomach and small intestine. In addition to reduced prostaglandin synthesis, COX inhibition in the GI tract also inhibits the production of gastric mucus and bicarbonate, cell proliferation, and the adequate flow of blood throughout the GI mucosa.
Several other factors appear to contribute to the pathogenesis of GI damage by ibuprofen. As lipid-soluble weak acids, ibuprofen and other NSAIDs act as a detergent when they encounter the phospholipid bilayer that lines the intestinal mucosa. By disrupting these cell membranes, NSAIDs increase intestinal permeability, which subsequently leads to intestinal inflammation and damage.
Cardiovascular effects
Ibuprofen, particularly when used at higher doses for extended periods of time, can increase the risk of several cardiovascular conditions, particularly heart attack and stroke.
Since 2019, the United States Food and Drug Administration (FDA) has enforced new warnings on ibuprofen and other NSAIDs regarding the cardiovascular toxicity risk of these drugs. These warnings state that ibuprofen, even when used in the short-term, can increase the risk of both heart attack and stroke, with the risk increasing with higher doses and longer duration of ibuprofen use. Individuals who already have heart disease are at a particularly high risk of these side effects.
Researchers believe that inhibiting endothelial prostaglandin I2 (PGI2) could be one of the possible mechanisms responsible for the cardiovascular disease risk associated with ibuprofen and other NSAID use, as PGI2 normally prevents thrombosis. Several other mechanisms have been hypothesized to contribute to the increased risk of cardiovascular disease associated with NSAID use; however, additional research is needed.
Renal toxicity
Various kidney complications have been associated with NSAID use, some of which include acute kidney injury (AKI) and chronic kidney disease (CKD). More specifically, the CKD complications associated with NSAID use include electrolyte imbalances, glomerulonephritis, renal papillary necrosis, fluid retention-induced hypertension, renal tubular acidosis, hyponatremia, and hyperkalemia.
 Image Credit: TanyaKim / Shutterstock
Image Credit: TanyaKim / Shutterstock
The renal toxicity of NSAIDs can occur with high doses or long-term use of these drugs. Current estimates indicate that about 2.5 million Americans each year experience renal complications as a result of their NSAID usage.
Prostaglandin-H-synthase 1 (PGHS-1) is synthesized in the collecting ducts and other cells within Bowman’s capsule of the kidney and has a vital role in regulating the glomerular filtration rate (GFR). Comparatively, PGHS-2, expressed within the epithelial cells that line the ascending loop and Henle and macula densa cells, maintains both sodium and water retention.
The inhibition of both PGH-1 and PGHS-2 by ibuprofen blocks prostaglandin production, thereby compromising normal GFR, which subsequently leads to ischemic injury and acute necrosis of the renal tubules. Prostaglandin inhibition also intensifies the renin-angiotensin-aldosterone pathway, which increases the reabsorption of sodium and increases the risk of both hypertension and edema.
Patients with preexisting severe hepatic or renal dysfunction, nephrotic syndrome with high-level proteinuria, older age, diabetes, hypertension, and congestive heart failure are at an increased risk of kidney toxicity due to ibuprofen usage.
High-risk populations
Patients with chronic pain, rheumatoid arthritis, osteoarthritis, and other musculoskeletal disorders are considered to be at an increased risk of the adverse effects of ibuprofen usage, particularly the renal toxicity associated with this drug. Furthermore, individuals over the age of 65 are also at an increased risk of NSAID toxicity, including acute renal failure.
Women taking ibuprofen should tell their doctor if they are pregnant or planning to become pregnant. Currently, the FDA advises that pregnant women avoid using NSAIDs like ibuprofen at 20 weeks or later in their pregnancy, as the use of these drugs by the mother may cause renal toxicity in the unborn baby. Ibuprofen appears in breast milk in extremely low concentrations and is generally regarded as safe for women to use while breastfeeding.
As ibuprofen and other NSAIDs are present in many combination medicines, people taking ibuprofen should consult their doctor or pharmacist before they use any other treatment for pain, allergies, or colds. Taking several products containing ibuprofen can increase their total dose consumption, subsequently increasing their risk of experiencing adverse effects.
Ibuprofen also interacts with several other drugs and can worsen the effect of those drugs. For example, ibuprofen interferes with the action of anticoagulant drugs like warfarin and can increase the risk of severe bleeding and fatal hemorrhage, especially within the GI tract.
In combination with corticosteroids, ibuprofen may also increase the risk of GI bleeding. Ibuprofen may also reduce the anti-hypertensive effects of angiotensin-converting enzyme (ACE) inhibitors, beta-blockers, and diuretics, thus increasing the risk of natriuresis and hyperkalemia in patients receiving these treatments.
Ibuprofen should not be taken with alcohol, as it significantly increases the risk of renal toxicity and other adverse effects.
Ibuprofen and Coronavirus (COVID-19)
References
- Ngo, V. T. H., & Bajaj, T. Ibuprofen. [Updated 2022 Jun 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK542299/.
- Ibuprofen (prescription) [Online]. Available from: https://www.arthritis.org/drug-guide/nsaids/ibuprofen.
- Ibuprofen Dosage [Online]. Available from: https://www.drugs.com/dosage/ibuprofen.html.
- Bjarnason, I., Scarpignato, C., Holmgren, E., et al. (2017). Mechanisms of Damage to the Gastrointestinal Tract from Non-steroidal Anti-Inflammatory Drugs. Gastroenterology 154(3); 500-514. doi:10.1053/j.gastro.2017.10.049.
- Hijos-Mallada, G., Sostres, C., & Gomollon, F. (2022). NSAIDs, gastrointestinal toxicity and inflammatory bowel disease. Gastroentereologia y Hepatologia 45(3); 215-222. doi:10.1016/j.gastre.2021.06.002.
- Side effects of ibuprofen [Online]. Available from: https://www.nhs.uk/medicines/ibuprofen-for-adults/side-effects-of-ibuprofen/.
- What is ibuprofen and how is it used? [Online]. Available from: https://www.versusarthritis.org/about-arthritis/treatments/drugs/ibuprofen/
- The Ibuprofen Risks You Need to Know [Online]. Available from: https://time.com/4746319/ibuprofen-painkillers-risks/
- FDA strengthens warning that NSAIDs increase heart attack and stroke risk [Online]. Available from: https://www.health.harvard.edu/blog/fda-strengthens-warning-that-nsaids-increase-heart-attack-and-stroke-risk-201507138138.
- Ibuprofen Pathway, Pharmacodynamics [Online]. Available from: https://www.pharmgkb.org/pathway/PA166121942
- FDA recommends avoiding use of NSAIDs in pregnancy at 20 weeks or later because they can result in low amniotic fluid [Online]. Available from: https://www.fda.gov/drugs/drug-safety-and-availability/fda-recommends-avoiding-use-nsaids-pregnancy-20-weeks-or-later-because-they-can-result-low-amniotic.
- Moore, N., Pollack, C., & Butkerait, P. (2015). Adverse drug reactions and drug-drug interactions with over-the-counter NSAIDs. Therapeutics and Clinical Risk Management 11; 1061-1075. doi:10.2147/TCRM.S79135.
Further Reading
Last Updated: Sep 14, 2022