The aim of treatment for periodontitis is to prevent damage to bones and connective tissue surrounding the teeth. A periodontist, dentist or hygienist usually does this by cleaning the pockets that have formed around the teeth so that the infection cannot spread.
There are various techniques that may be indicated depending on the specific case, including both non-surgical and surgical techniques. In severe cases, the treatment may last for many years.
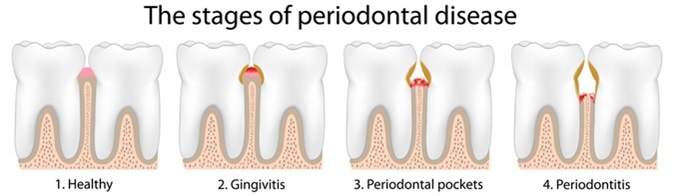
Periodontal Disease Stages - Image Credit: Alila Medical Media / Shutterstock
Non-Surgical Treatments
For mild to moderate cases of periodontitis, it is often possible to treat it using with minimally invasive dental procedures, without the need for surgery. This may include techniques such as:
- Scaling of the teeth to remove bacteria and tartar from the surface of the teeth and underneath the gums. There are several instruments that may be used to perform this, such as a laser or ultrasonic device.
- Root planing to smooth the surface of the roots of the teeth and help to prevent additional buildup of tartar in the area. This can also help to remove the byproducts of bacterial infection, which can cause inflammation and delay healing.
- Antibiotics to control the bacterial infection in the area. Topical antibiotics in a month rise or gel or oral systemic antibiotics may be recommended, depending on the cause and extent of infection.
Surgical Treatments
In some cases, dental surgery may be required to treat periodontitis. There are various surgical techniques that may be indicated, such as:
- Flap surgery to reduce the size of pockets in the gums, because large flaps can increase the risk of the bone becoming infected. This involves making small incisions in the gum so that the tissue can be lifted back to allow the roots to be exposed for scaling and root planning.
- Soft tissue grafts to reduce additional recession of the gums and cover any exposed roots, thus improving the aesthetics of the mouth. This involves the removal of healthy tissue from another area of the mouth, such as the palate, or from a donor, which can then be attached to the affected site to replace lost tissue.
- Bone grafting to prevent tooth loss by supporting the placement of the tooth and to encourage the regrowth of natural bone. This involves the attachment of bone to the affected area, either from fragments of the patient bone, donated bone or synthetic bone.
- Guided tissue regeneration to prevent unwanted tissue from growing over the area and allow the regrowth of bone. This involves the placement of a biocompatible fabric between the bone and the tooth.
- Tissue-stimulating proteins to stimulate the growth of health bone and connective tissue in the area. This involves the application of a gel that contains certain proteins to the root of a diseased tooth.
Ongoing Management
It is important for patients who are or have been affected by periodontitis to implement changes to their dental hygiene to help prevent recurrence of the condition.
Patients should be recommended to implement good oral hygiene practices, such as brushing the teeth twice a day and flossing daily. People who use tobacco or smoke should also be advised to quit as smoking can reduce the efficacy of treatment and increase the likelihood that the disease will recur.
Additionally, patients affected by periodontitis should be advised to schedule regular follow-up appointment to monitor the progression of the disease and implement action when necessary.
References
Further Reading
Last Updated: Feb 27, 2019