Authors Jack A. Gilbert of the University of California San Diego and Erica M. Hartmann of Northwestern University found that while oral microorganisms may enter the gastrointestinal tract and contribute to gut dysbiosis, the mechanisms and broader implications of these interactions require further study.
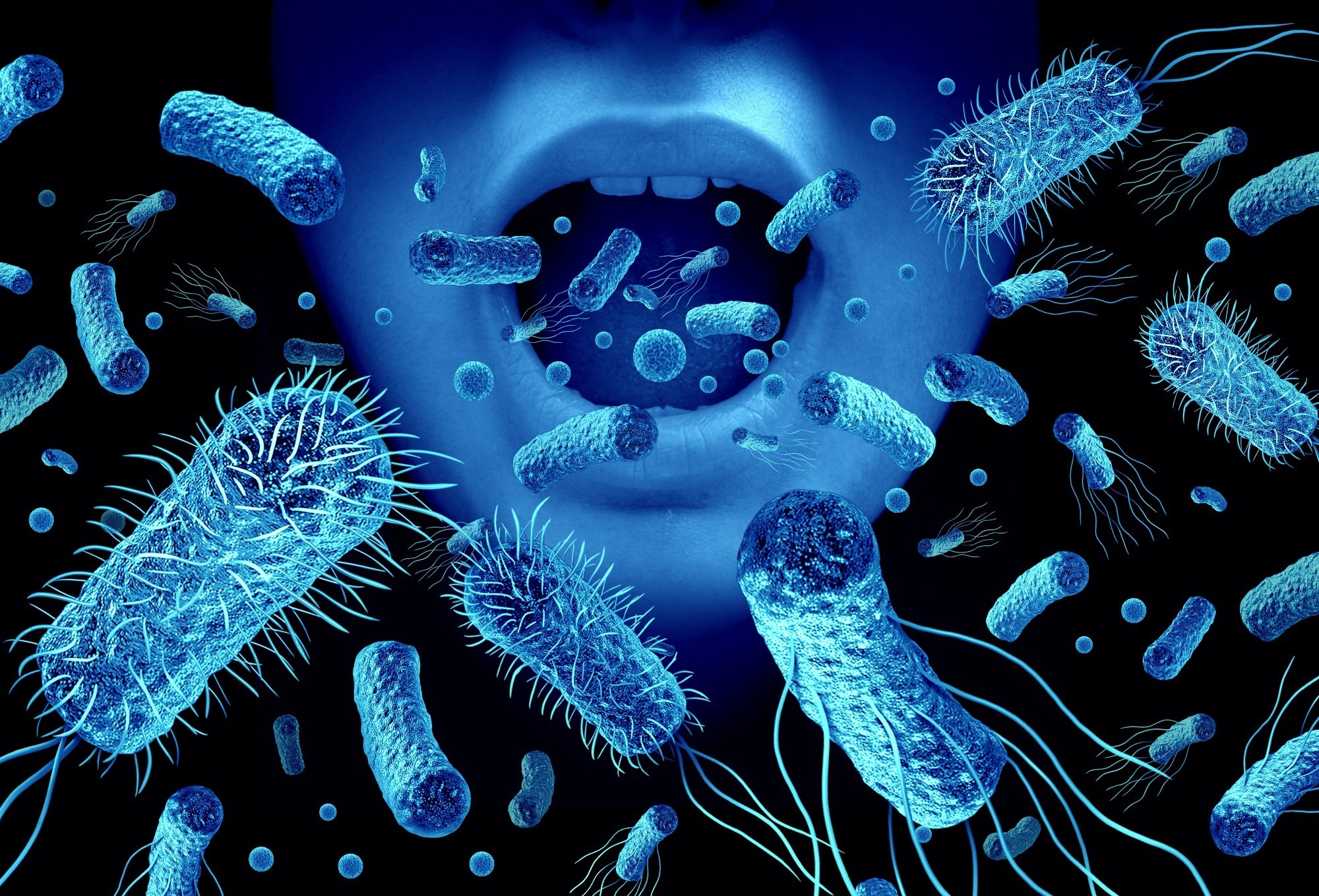 Review Article: The indoors microbiome and human health. Image Credit: Lightspring / Shutterstock
Review Article: The indoors microbiome and human health. Image Credit: Lightspring / Shutterstock
The importance of the gut microbiome
The human body hosts a vast diversity of microorganisms that play a vital role in health by supporting the immune system and defending against pathogens. However, they may also contribute to chronic diseases.
Dysbiosis, or disruptions in these microbial communities, is linked to metabolic and autoimmune disorders and gastrointestinal issues. The gut and oral cavity are two key areas with dense microbial populations.
The oral microbiome is influenced by food and environment and has been linked to oral diseases like gingivitis and periodontitis, affecting systemic health by influencing microbial populations in the digestive and respiratory systems.
The gut microbiome, shaped by genetics, diet, and lifestyle, is crucial for immune responses and infection prevention. Understanding the interactions between the gut and oral microbiomes is necessary for grasping their impact on diseases like colorectal cancer (CRC) and inflammatory bowel disease (IBD).
The oral cavity is a gateway
The gastrointestinal tract begins at the mouth and extends to the anus, including organs like the liver, pancreas, and gallbladder. The oral cavity, highly vascularized and home to diverse microbial communities, serves as the primary entry point for microbes into the body.
It hosts over 770 bacterial species in different microenvironments, such as the buccal mucosa, tongue, and dental plaques. Key genera include Streptococcus, Veillonella, and Prevotella. The gut microbiome, primarily anaerobic and comprising species like Bacteroides and Ruminococcus, shares some taxa with the oral cavity, but distinct physical and chemical barriers usually prevent oral microbes from colonizing the gut.
However, under conditions like low gastric acidity or antibiotic use, oral bacteria can migrate to the gut, potentially contributing to diseases. Understanding this oral-gut microbial transfer is crucial for exploring its role in disease and health.
The mouth-gut connection
The oral cavity, susceptible to conditions like dental caries, oral cancers, and periodontal diseases (gingivitis and periodontitis), plays a significant role in overall health. Periodontal diseases involve the destruction of tissues around the teeth due to an inflammatory response to plaque and microbes.
Gingivitis, a reversible inflammation of the gums, can progress to periodontitis if untreated, causing deeper tissue damage and bone loss. Research suggests a strong link between oral health and gut diseases.
Periodontal pathogens, such as P. gingivalis and F. nucleatum, can migrate from the mouth to the gut, contributing to conditions like IBD. These bacteria promote inflammation and disrupt the gut’s microbial balance.
Studies have found higher levels of oral bacteria in the guts of individuals with IBD, indicating the mouth-gut axis’s role in these diseases. Additionally, the oral microbiome has been associated with CRC. Oral bacteria like F. nucleatum can influence tumor growth and treatment resistance in CRC.
This connection underscores the importance of oral health in preventing and managing systemic diseases. Understanding these links can lead to better prevention and treatment strategies for gut diseases and cancers.
Oral health and overall health
Poor oral health, especially periodontitis, can significantly impact the entire body. Oral bacteria can travel through the gastrointestinal tract and bloodstream, contributing to various diseases.
Periodontitis causes low-grade systemic inflammation, which can disrupt the body’s health and promote diseases like IBD and cardiovascular diseases. It increases levels of pro-inflammatory cytokines in the blood, indicating an ongoing inflammatory response.
One mechanism through which oral health affects the body is through the bone marrow, where inflammation from periodontitis boosts the production of immune cells, leading to heightened inflammatory responses elsewhere.
Another mechanism involves periodontal bacteria directly affecting distant organs by releasing toxins that promote inflammation and diseases like rheumatoid arthritis and atherosclerosis. Additionally, oral health impacts the gut directly. Bacteria from the mouth can colonize the gut, exacerbating conditions like IBD.
Treating periodontal disease can reduce systemic inflammation and improve chronic disease symptoms, demonstrating the bidirectional relationship between oral health and systemic diseases. Addressing oral health is thus crucial for overall health and managing systemic conditions.
Conclusions
Changes in oral bacteria can affect gut health, leading to systemic inflammation and various diseases. The relationship between the oral cavity and gut is bidirectional, but the exact mechanisms remain unclear.
More research is needed to understand how oral bacteria influence chronic diseases and to develop better models for studying these interactions. Future studies should resolve the oral-gut microbiome axis at the strain level to confirm the role of oral bacteria in chronic diseases and examine the role of translocated strains in gut microbiome-linked diseases through in vivo and in vitro models.