Mechanics of insulin pumps: Precision delivery for blood sugar control
Understanding basal rates and bolus doses
Clinical and lifestyle benefits of insulin pump therapy
Key factors in choosing and using an insulin pump
Advances shaping the future of insulin pump technology
References
Further reading
With the prevalence of diabetes quadrupling in recent decades and currently impacting more than 500 million people in the world, it is no surprise that the technology for insulin delivery has also evolved.1,2
An insulin pump is a cell phone-sized wearable device that carries a reservoir of insulin for the user. This device is programmed to dispense specific volumes of insulin automatically when consuming food.3
While the first commercial insulin pump reached the market in the 1970s, its rapid uptake by users only occurred from the early 2000s, with the Diabetes Control and Complication Trial (DCCT) in the early 1990s demonstrating the significance of intensive insulin therapy for optimum glycemic control and avoid complications related to diabetes.4
Since its uptake, insulin pumps have been shown to be an innovative alternative to multiple daily insulin injections for those with diabetes who require insulin to manage their condition.5
Additionally, users of insulin pumps have their basal insulin constantly delivered without worrying about remembering to inject their insulin, with the device having the capacity to be programmed to deliver a higher amount of insulin at particular times during the day or even during sleep.3
Mechanics of insulin pumps: Precision delivery for blood sugar control
There are three main components of insulin pumps: (i) the pump, (ii) the infusion set, and (iii) the sensor and transmitter in sensor-augmented insulin pumps.2
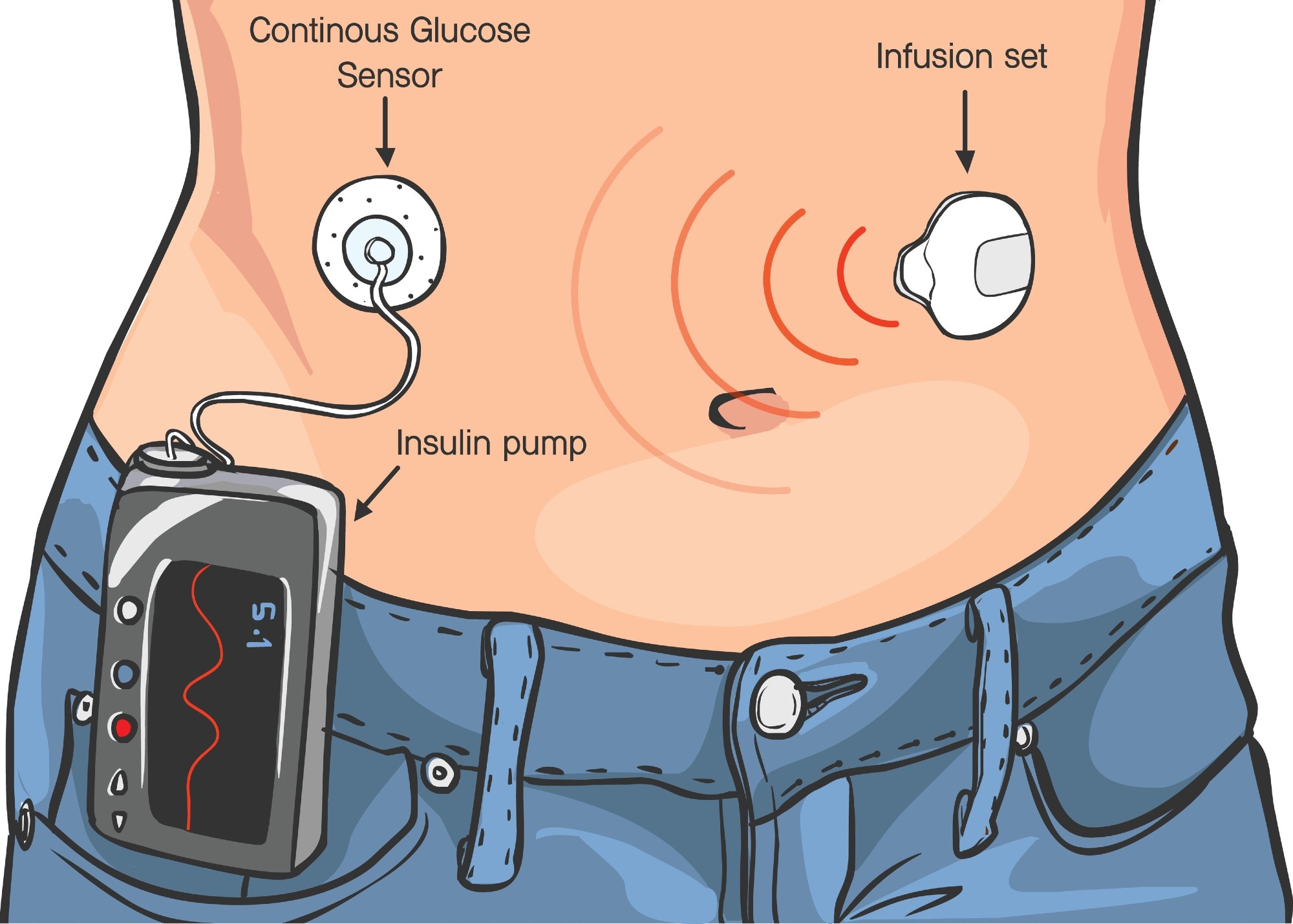 An insulin pump system featuring a continuous glucose sensor to monitor blood sugar levels, an infusion set to deliver insulin, and a pump device for precise diabetes management.
An insulin pump system featuring a continuous glucose sensor to monitor blood sugar levels, an infusion set to deliver insulin, and a pump device for precise diabetes management.
Most devices consist of a pump and infusion set that are separate from each other, with a connecting plastic tube; however, some devices combine both of these components without the requirement of a tube – this is known as a tubeless pump.2
Tubed insulin pumps utilize a long and thin tube that connects the pump to a cannula under the skin to deliver insulin to individuals. A tubed insulin pump is usually constructed with durable plastic and metal, with an interactive screen for viewing and modifying various settings. It also consists of a cartridge or reservoir of insulin with a replaceable or rechargeable battery.5
Most reservoirs require changing every two to three days or once the insulin runs out.2 Most components of the device, such as the reservoirs and tubing, are replaced, but the pump itself usually lasts for many years.5
However, tubeless insulin pumps, such as patch pumps, use a flexible plastic tube or cannula under the skin, with the insulin reservoir and cannula being part of one “pod” that sits on the skin with the aid of an adhesive patch. This category of devices does not utilize an external tube, and the pump is managed using a handheld wireless controller.5
This type of pump consists of the user filling the reservoir with insulin before attaching the pod and fixing the adhesive to the skin. A button is then pushed to release a needle that is threaded through the cannula in the pod, which is retracted back into the pod and remains under the skin.5
Understanding basal rates and bolus doses
Insulin pumps mimic the way the pancreas naturally releases insulin in two different ways.5
The first way is through basal insulin, consisting of small and continuous insulin doses. Most pumps deliver basal rates that the user and their healthcare provider manually program.5 This consists of the insulin being continuously delivered at a preset or auto-adjusted rate for a basal supply, which lasts for 24 hours.2,5
Basal rates require changing over time as the body and routines change, which would need adjustment with the help of a healthcare provider. All pumps can automatically adjust basal doses dependent on an individual’s glucose levels, which are monitored via a connected continuous glucose monitoring (CGM) program.5
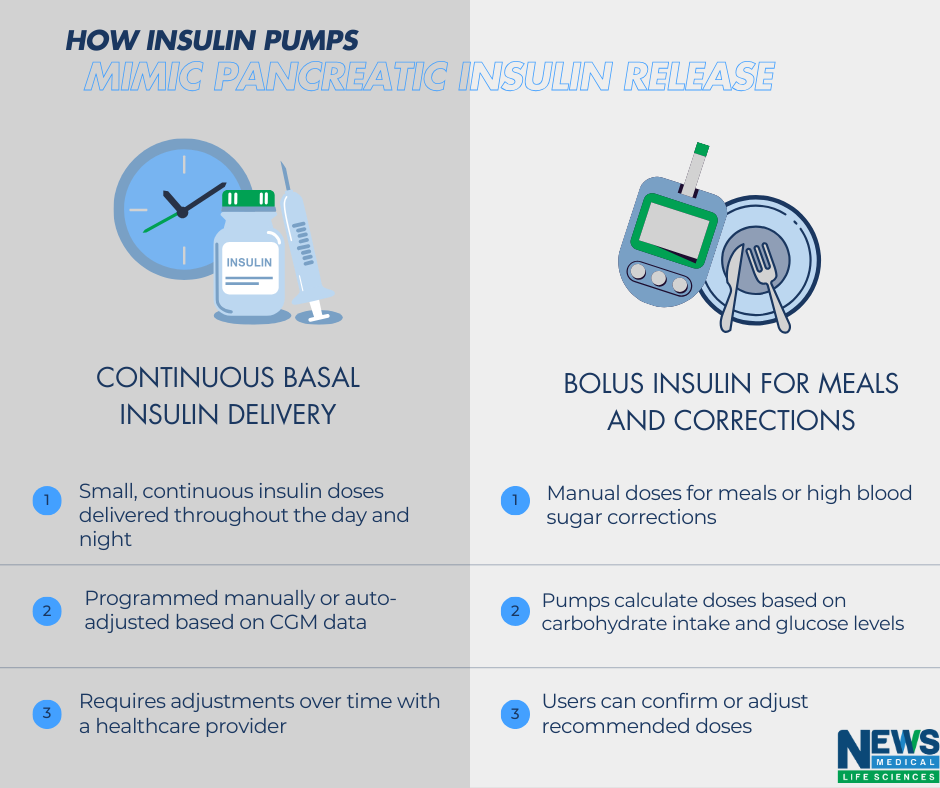
Image Credit: News-Medical.net
Another way pumps work is through bolus doses, including manual increases of insulin when eating or to correct high blood sugar. Pumps utilize information entered about carbohydrate intake and blood sugar levels to calculate how much bolus insulin is required. A majority of pumps provide a recommended dose that a user can either confirm or adjust before delivering insulin.2,5,7
Clinical and lifestyle benefits of insulin pump therapy
Insulin pumps deliver continuous insulin with a flexible and precise approach to managing a diabetes diagnosis. There are many benefits of using an insulin pump compared to traditional management methods such as insulin injections.8
Insulin pumps offer improved glycemic control as the continuous delivery of insulin and precise adjustment enable users to have more stable blood glucose levels.4 Subsequently, this decreases the risk of hyperglycemia, also known as high blood sugar, as well as hypoglycemia or low blood sugar.8
Additionally, insulin pumps can also provide a higher level of flexibility and freedom in lifestyle choices, including meal timing, exercise, and travel, without the thought of having to inject insulin depending on the activity.4,8 However, with the use of injections, any changes to basal insulin require careful planning several hours in advance.6
Insulin pump users can easily adjust and modify insulin delivery for various activities, including spontaneous events, leading to an increased quality of life and a sense of control over their diabetes management.8
A statistical study reported the most common insulin-related errors, which included missed doses of insulin (25%), timing errors (22.7%), and missed documentation of insulin doses (15.5%).1 With these in mind, the use of an automated insulin delivery system, such as through an insulin pump, may be more beneficial to mitigate the risks of missed doses.8
While an insulin pump can cost approximately $6000 in the United States, with the supplies costing between $3000 to $6000 yearly, patients who switch from multiple-dose insulin injections to pumps in a managed care setting have seen a reduced insulin expenditure by approximately $657 per year.9
Key factors in choosing and using an insulin pump
Many insulin pumps are integrated with continuous glucose monitoring (CGM), which continuously tracks glucose levels in real-time, enabling automated insulin adjustments and alerts and enhancing overall glucose management.8
However, while pumps are advanced devices, there are some drawbacks and considerations, such as the cost of insulin pumps and their supplies, which can be expensive and act as a barrier for many individuals unable to afford these devices.8
Additionally, there is also a need for ongoing education and support required for users of insulin pumps in order to be able to manage the device effectively. This can be a limitation for some who may find the technology to be overwhelming or complicated.8
Potential complications with insulin pumps also include technical issues and malfunctions, as with any electronic device, which requires users to be prepared to troubleshoot these issues and carry backup supplies and insulin.8
Regular pump site care is also required, as the infusion site can occasionally result in irritation, discomfort, or infection.8
Other complications of the pump also include the risk of diabetic ketoacidosis (DKA), as insulin pumps deliver rapid-acting insulin, and so if the pump fails or if there is an obstruction in delivering insulin, this can lead to DKA.8
Advances shaping the future of insulin pump technology
The transformation of glucose management methods has also expanded using artificial intelligence (AI), with this realm introducing innovative strategies. This evolution included transitioning from using pumps based on proportional integral derivative (PID) controllers to using a model based on a predictive control (MPC) approach. MPC utilizes dynamic models to predict future behavior and consider current control inputs.10
Personalized models are also evolving continuously to predict immediate blood glucose events as well as long-term glucose trends through the use of individual blood glucose data, with a high level of accuracy and a margin of error of 10%.10
With advancements in this area of medical devices, newer and more refined technologies aim to have better ease of use and quality of care, which leads to improved glycemic control.2
References
- Thota S. Insulin. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK560688/#:~:text=The%20insulin%20pump%20is%20a%20device%20that%20works,short-acting%20insulin%20to%20the%20body%20throughout%20the%20day. Published July 10, 2023. Accessed December 2, 2024.
- Yao PY. Insulin Pump. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK555961/. Published August 28, 2023. Accessed December 2, 2024.
- Insulin Pump. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/type-1-diabetes/multimedia/insulin-pump/img-20006962. Accessed November 25, 2024.
- Berget C, Messer LH, Forlenza GP. A clinical overview of insulin pump therapy for the management of diabetes: Past, present, and future of intensive therapy. Diabetes Spectrum. 2019;32(3):194-204. doi:10.2337/ds18-0091. https://pmc.ncbi.nlm.nih.gov/articles/PMC6695255/
- Types of Insulin Pumps. Cleveland Clinic. https://my.clevelandclinic.org/health/articles/insulin-pumps. Published November 12, 2023. Accessed November 25, 2024.
- Singh A. Multiple Insulin Injections Vs Insulin Pumps. Diabetes. https://www.diabetes.co.uk/insulin/mdi-vs-insulin-pumps.html. Published October 29, 2023. Accessed November 25, 2024.
- Yeh T, Yeung M, Mendelsohn Curanaj FA. Managing patients with insulin pumps and continuous glucose monitors in the hospital: To wear or not to wear. Current Diabetes Reports. 2021;21(2). doi:10.1007/s11892-021-01375-7. https://pubmed.ncbi.nlm.nih.gov/33449214/
- Lorenyz C. Insulin Pump Therapy for Glycemic Control: Benefits and Potential Drawbacks. Diabetes Management. 2024;14(4):642-643. doi:10.37532/1758-1907.2024.14(4).642-643. https://www.openaccessjournals.com/articles/insulin-pump-therapy-for-glycemic-control-benefits-and-potential-drawbacks.pdf
- McAdams B, Rizvi A. An overview of insulin pumps and glucose sensors for the generalist. Journal of Clinical Medicine. 2016;5(1):5. doi:10.3390/jcm5010005. https://pubmed.ncbi.nlm.nih.gov/26742082/
- Yu TS, Song S, Yea J, Jang K. Diabetes management in transition: Market insights and technological advancements in CGM and insulin delivery. Advanced Sensor Research. 2024;3(10). doi:10.1002/adsr.202400048. https://onlinelibrary.wiley.com/doi/10.1002/adsr.202400048
Further Reading
Last Updated: Dec 11, 2024