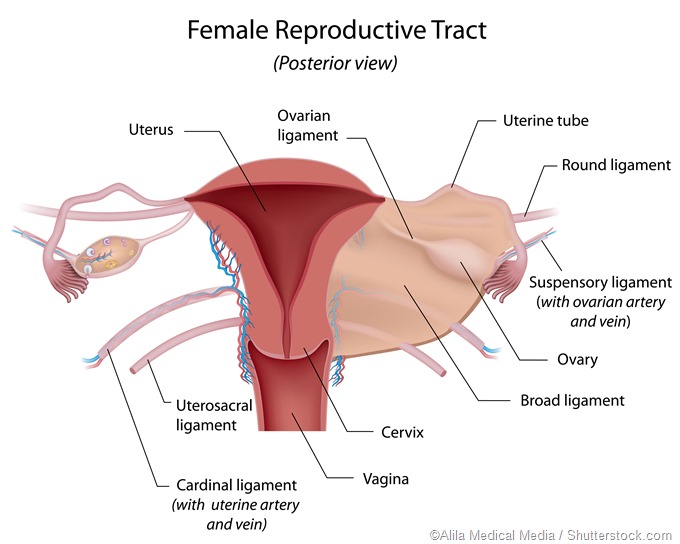
Pelvic inflammatory disease (PID) is a term used to describe the inflammation of the upper genital tract that involves the fallopian tubes and ovaries. As the majority of PID cases are a result of ascending or blood-borne infections, the process is often bilateral (although one tube may be more gravely affected than the other). The inflammation can also extend to the parametrium and the pelvic peritoneum – either simultaneously or subsequently.
The impairment of the natural protective mechanism
In normal circumstances there are several natural barriers that prevent the ascent of pathogenic microorganisms from the vagina to the fallopian tubes. Moreover, the intact hymen successfully prevents ascending infection, so when a virginal girl presents with PID, a potential tubercular spread must be considered.
The acidity of the vaginal secretions has the propensity to inhibit the growth of bacteria, while the cervical canal has a relatively small lumen and is filled with a plug of alkaline mucus. The ciliary movement existing in the endometrial lining of the uterus and cervical canal is also aimed downwards, which discourages the upward expanse of otherwise non-motile microorganisms to the uterus.
Such natural protective mechanisms are impaired during menstruation, but also after delivery or abortion, since the cervical canal becomes dilated, the vaginal pH increases, and the protective epithelial lining of the endometrium is shed. All of that renders the genital tract more vulnerable and prone to infection.
In addition to aforementioned factors, various intrauterine manipulations (such as curettage or manual removal of placenta) favor entry and subsequent spread of pathogenic microorganisms. Intrauterine devices (IUD) which are used as contraception for women may also represent a source of infection, most notably when they are not introduced under aseptic conditions or when there was a prior presence of vaginal infection.
Sexually transmitted infections as the most common cause
Before the 1970s it was believed that PID was a monoetiologic infection caused primarily by the gram-negative coccus Neisseria gonorrhoeae. Nevertheless, subsequent studies that utilized laparoscopy and endometrial aspirations to retrieve material from the upper genital tract demonstrated that the etiology of acute PID is actually polymicrobic in nature with a panoply of microorganisms that can be implicated.
In addition to Neisseria gonorrhoeae, one of the most common causative factors is another sexually transmitted agent – obligate intracellular pathogen Chlamydia trachomatis. Mathematical modeling based on relevant microbiological and epidemiological studies suggests that up to 10 percent of women infected with chlamydia may develop PID if left untreated. In addition, gonococci and chlamydia create a milieu for secondary invasion by other organisms.
The damage of fallopian tubes in the context of infection with Chlamydia trachomatis appears to be linked both to an innate immune response sparked by the infected epithelial cells and to an adaptive T-cell immunity. Still, even though antibodies specific for chlamydial antigens are boosted in severe disease, higher titers are not closely correlated with worse reproductive outcomes.
Some other sexually transmitted agents also play a certain role in the pathogenesis of this disease. Mycoplasma hominis is isolated in 50 percent of sexually active women, but found in only 7 percent of those with PID. On the other hand, Mycoplasma genitalium has been more closely associated with PID, though the prevalence of this bacterium is low in the majority of studied populations.
Other microorganisms and subclinical pelvic inflammatory disease
A large number of non-sexually transmitted pathogens (i.e. non-chlamydial and non-gonococcal microorganisms) can be found in the upper genital tract of women with acute PID. They are closely associated with bacterial vaginosis – this is a complex disruption of the vaginal flora that leads to the loss of lactobacilli that normally produce hydrogen peroxide, and the overgrowth of Gardnerella, Mobiluncus, Prevotella, alpha-hemolytic streptococci and black-pigmented anaerobic rods.
Multiple research groups have shown an association between bacterial vaginosis and acute PID. Furthermore, the usage of modern molecular techniques to determinate uncultivable bacteria has identified genetic sequences of anaerobic bacteria linked to bacterial vaginosis in the fallopian tubes of women with confirmed acute PID.
Subclinical PID is a term that was originally applied to women with known tubal factor infertility linked to chronic inflammatory residua specific for PID, but without a history of diagnosis or treatment for acute PID. In any case, agents associated with this type of pelvic inflammatory disease are the most common putative microorganisms, such as Neisseria gonorrhoeae and Chlamydia trachomatis.
Further Reading
Last Updated: Feb 27, 2019