Pelvic inflammatory disease (PID) is a term used to describe the infection and inflammation of the upper genital tract in women, commonly involving the ovaries, fallopian tubes and surrounding structures. It is a frequent and serious complication of certain sexually-transmitted diseases, most notably chlamydia and gonorrhea.
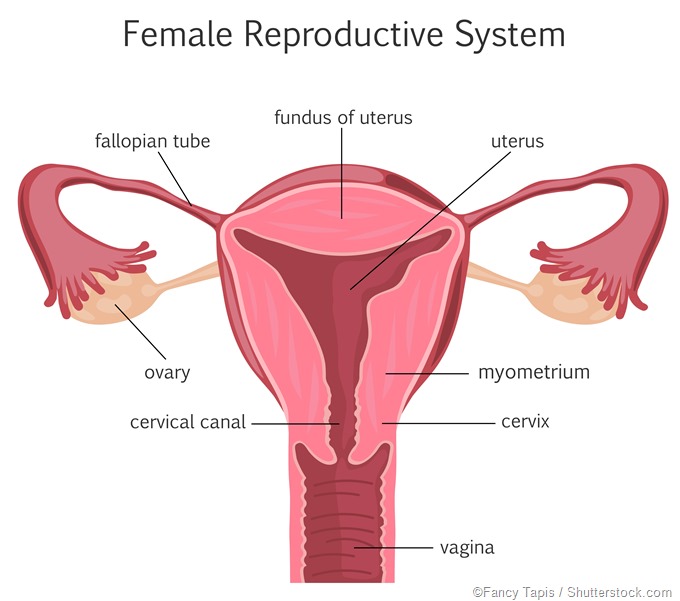
Physicians should always be aware of PID and initiate treatment in all women at risk that present with uterine, cervical or adnexal motion tenderness during bimanual examination. The end-goal is to adequately treat the infection, minimize tubal damage and prevent adhesions, avoiding in turn looming sequelae of tubal damage.
Antibiotic treatment
Any damage to the female reproductive tract that arises as a result of PID is most often irreversible; hence, timely antibiotic treatment is of uttermost importance to prevent scar development. In any case, treatment regimens for this clinical entity must consist of empiric and broad spectrum coverage of pathogens that are likely implicated in its development.
Different oral and parenteral antimicrobial regimens have shown comparable efficacy in women presenting with mild or moderately-severe PID. In more severe cases initial therapy is usually parenteral, but clinical experience should guide a further decision-making whether a transition to oral therapy should be pursued (most often within 24 to 48 hours of clinical improvement).
The decision to hospitalize patients with PID should be based on the clinical judgement of the provider. However, inpatient hospitalization for treating this condition is not considered economically feasible, thus the US Centers for Disease Control (CDC) recommendations are supporting oral regimens in the outpatient setting whenever feasible.
On the other hand, inpatient treatment is advocated for women who meet certain criteria, such as the inability to clinically exclude a potential surgical emergency, pregnancy, the presence of tubo-ovarian abscess, severe illness (characterized by vomiting and high fever), inability to follow a proposed outpatient regimen, as well as failure to respond to prescribed oral antibiotics with persistent or worsening symptoms.
In addition, all patients who received the treatment should be reevaluated by an attending clinician within 72 hours in order to assess the clinical status of the affected individual – this is especially important, taking into account the rise of multidrug-resistant Neisseria gonorrhoeae. Considering the latter, it must be noted that the spread Neisseria gonorrhoeae resistant to cephalosporin antibiotics is estimated to cause an additional 75 thousand cases of PID during a 10-year period.
Surgical approaches
Surgery may be warranted in cases of acute spreading peritonitis, intestinal obstruction and ruptured tubo-ovarian abscess (which are considered complications of PID), but also when treating pelvic abscesses by posterior colpotomy or evacuating septic products of conception. Furthermore, chronic PID necessitates surgical treatment since there is always some kind of pelvic pathology following the acute infection.
In cases of tubo-ovarian abscess minimal invasive surgery may also be a choice if the abscess fails to respond to antibiotics in 48-72 hours, if it ruptures, or if pyoperitoneum develops. Such procedures have the advantage of minimal ovarian tissue damage in young women, albeit adequate follow-up is essential.
Laparoscopic breaking of external adhesions (either by electrocauter or by laser) is indicated if the tubal blockage is due to external adhesions. Furthermore, cannulation or hysteroscopic balloon catheter-plasty are successful if the blockage us due to luminal detritus or mild stricture.
Prognosis of pelvic inflammatory disease
The prognosis of PID depends mostly on the awareness of adolescents to look for timely health care and to prevent future episodes of sexually-transmitted infections. Each episode of PID, depending on the degree of severity, opens the door for the potential development of complications, with infertility as the most striking example. In light of this, sexually active women (especially in adolescence) who have had PID before should also undergo active screening for sexually-transmitted infections.
The use of barrier contraceptives, adherence to proper asepsis during instrumental manipulations and swift treatment of suspected infections are still the top-notch approaches for safeguarding the patient from infections that may result in PID. There are also female condoms which cover the cervix, entire vagina and the external genitalia that may be used for protection against sexually-transmitted infections.
In conclusion, behavioral interventions that are designed to enhance physician and patient adherence to treatment guidelines were shown to work, but in order to improve population outcome they must be implemented widely. The need for vigilant screening for asymptomatic sexually-transmitted pathogens in women at risk is key in preventing PID.
Further Reading
Last Updated: Dec 29, 2022