Polycystic ovary syndrome (PCOS) is a disorder which may present in different ways, and affects about 5-8% of women of reproductive age in the USA.
It is characterized by the presence of menstrual irregularities, chiefly anovulatory in origin, hirsutism acne, low fertility and hyperandrogenism. Its prevalence varies with region, and may depend upon racial, dietary, lifestyle and genetic factors, as well as the criteria for its diagnosis, which may change from place to place.
The metabolic syndrome is a group of metabolic dysfunctional features, including abdominal obesity, insulin resistance, hyperglycemia due to impaired glucose metabolism, high blood pressure, and abnormal blood lipid levels.
Both serum triglycerides and HDL cholesterol are affected, being increased and decreased respectively. In consequence, this group is at increased risk of developing type 2 diabetes mellitus, cardiovascular disease including coronary heart disease, and endometrial or womb cancer.
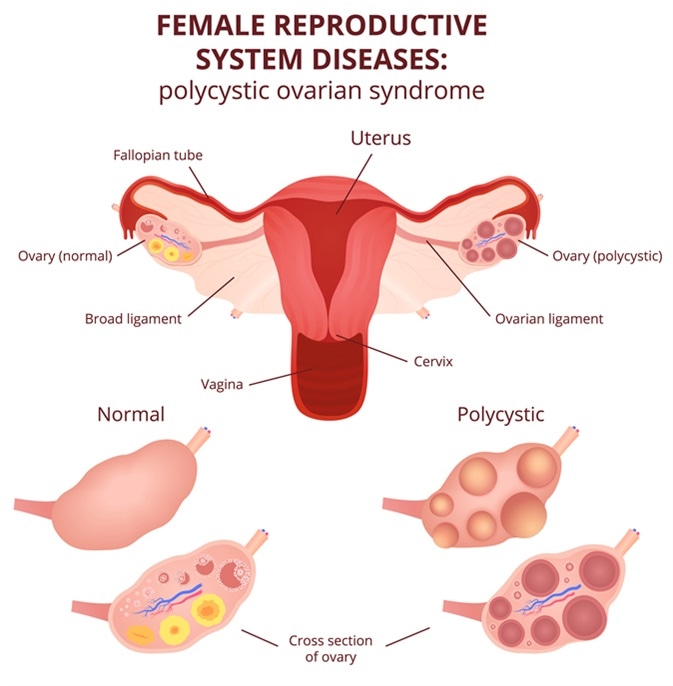
Female reproductive system, the uterus and ovaries scheme, polycystic ovary syndrome, ovarian cyst. Image Credit: Marochkina Anastasiia / Shutterstock
Risk Factors
Visceral obesity
These syndromes are clearly interrelated because many patients with PCOS have a large waistline, poor glucose tolerance and high insulin resistance resulting in increased insulin levels.
Almost half of them have the metabolic syndrome and share the health risks. In other words, the risk of metabolic syndrome is increased 11 times in women with PCOS.
Women with PCOS and gross obesity have a 14-fold increase in risk for metabolic syndrome. This is significant because those who did not meet the criteria for obesity did not have metabolic syndrome either. Visceral adipose tissue has a unique metabolism which is involved in the genesis of hyperinsulinemia.
This overlap cannot be ascribed solely to the common factor of a high BMI because even without such obvious visceral obesity or high cholesterol levels, women with PCOS still have a fourfold risk of metabolic syndrome.
Even patients with PCOS in whom ovulation still occurs have a twofold risk. This means that PCOS may be the leading risk factor for cardiovascular disease in young women.
Conversely, women suffering from infertility as a result of PCOS have an increased incidence of PCOS compared to age-matched controls.
Hyperinsulinemia
Women with PCOS and metabolic syndrome have a fasting insulin level which is, on average, twice as high as that in women who have PCOS but not metabolic syndrome.
This is important because insulin resistance is a key component of the dangerous metabolic changes in this syndrome, as it causes a compensatory rise in the insulin secretion, affecting other metabolic functions negatively.
Thus hyperinsulinemia is the link between these two syndromes, and the primary reason for the increased cardiovascular risk in women with PCOS and metabolic syndrome.
SHBG levels
The levels of SHBG (sex hormone binding globulin) may vary with the BMI and level of insulin resistance, being related to the hepatic suppression of production of this protein, triggered by hyperinsulinemia.
A low SHBG is therefore a possible marker for insulin resistance.
Dr Neena Malhotra with Dr KK Aggarwal on How PCOS is different from metabolic syndrome
Diagnosis and Treatment
All women with PCOS who have a high BMI should undergo screening for metabolic syndrome. Even if this is negative, it should be performed regularly, every 2-3 years, to ensure that metabolic syndrome, if it occurs, is caught early enough to effectively reduce the cardiovascular risk.
All women who screen positive should be treated by lifestyle modification, and only beginning medication if failing to achieve this.
Weight reduction through dietary changes and exercise are key in this process. Oral contraceptives may help in reducing hyperandrogenism and acne, as well as helping to ensure regular menstrual cycles. Ovulation induction using clomiphene may be indicated if pregnancy is desired.
Metformin is an insulin sensitizer and may be helpful in managing the prediabetic stage. Dyslipidemias refractory to weight loss may require statin therapy.
All interventions should be aimed at bringing down insulin levels, as this benefits both conditions.
Further Reading
Last Updated: Feb 27, 2019