Quadriceps tendon rupture is a relatively rare injury which should be diagnosed early and treated promptly by surgery.
Causes
Most quadriceps tendon injuries are known to have been caused by direct impact or forced knee flexion due to falls, which account for about 62%, while spontaneous ruptures are uncommon, seen in only 3%. 88% of such ruptures occur in patients over 40 years.
The site of injury is typically within 1-2 cm of the upper end of the kneecap, at the junction of the tendon with the bone.
Risk factors include age over 40 years (with peak incidence in the fifties) because of decreased vascularity, or the presence of medical conditions such as gout, diabetes, rheumatoid arthritis, systemic lupus erythematosus, hyperparathyroidism or end-stage renal disease. Long-term corticosteroid use and gender (males are affected eight times more commonly) are other factors. The non-dominant limb is known to have suffered this injury twice as often as the other in a series of patients.
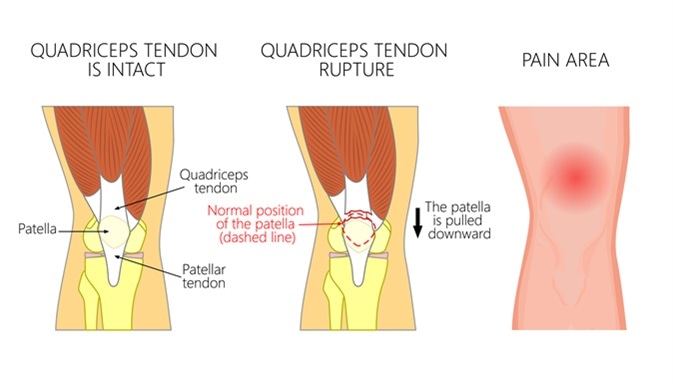
Quadriceps tendon rupture problem. Anatomy, front view of the human knee. Image Credit: Aksanaku / Shutterstock
Symptoms
Quadriceps tendon rupture is usually signaled by acute pain in the affected limb, and inability to extend the knee on that side, usually following a direct injury. When it results from an indirect trauma, it is because of microtraumas repeated over a period of time which have caused tendinitis or jumper’s knee, predisposing to rupture.
Diagnosis and Management
Diagnosis is based on the clinical history and symptoms including the feeling of a gap in the tendon above the knee. Imaging may be helpful to confirm the condition and rule out other injuries. Observing the swiveling of a needle inserted into the tissue above but not within the distal 5 cm of the tendon above the kneecap, may help in precise identification of the occurrence of such ruptures, and facilitate early treatment.
In most cases, patella drill holes are used to repair the torn tendon, while simple suturing techniques are applied in cases where the mid-substance is torn. If the tendon ends have retracted from the site of injury, or are ragged, reinforcement techniques are used. Following reattachment of the torn ends, the limb is placed in a cast for about 3-10 weeks, depending on other injuries and the severity of the tear.
Results have been almost identical across the spectrum of surgical repair techniques. The initial quadriceps muscle strength assessment shows atrophy to be present, which is worse in cases where the repair has been delayed. Surgical repair is preferred to non-surgical treatment because of the higher incidence of tendinitis in the latter, which is usually employed in cases of incomplete rupture. This is thought to be because all the damaged tissues do not heal equally, instead they become fibrosed or inflamed.
Outcomes and Complications
While uncommon, complications include heterotopic ossification, deep vein thrombosis, pulmonary embolism, infection of the overlying skin and subcutaneous tissue, and deep infection. Ultimately, however, the range of movement at the joint gets restored to within two degrees of the other limb post-repair, while repeat rupture is seen to occur in only 2%. Most patients resume the pre-injury level of physical activity after 18 weeks on an average. This is usually true irrespective of the technique of repair used, if it is performed within a week of tendon rupture.
Further Reading
Last Updated: Feb 27, 2019