Rotavirus represents the leading cause of severe childhood gastroenteritis. Every year rotavirus is thought to be responsible for approximately 25 million clinic visits, two million hospital admissions, and more than 800,000 deaths in children under the age of five globally. Although this disease has a worldwide distribution, most deaths occur in developing countries.
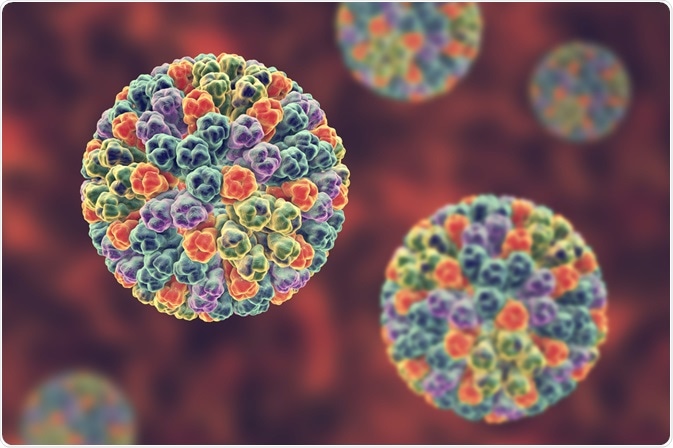
Image Credit: Kateryna Kon / Shutterstock.com
It is hard to distinguish gastroenteritis caused by rotavirus from other enteric pathogens. Therefore, establishing an adequate diagnosis requires testing of fecal specimens with commercially available assays. Still, rotavirus is not routinely sought in patients with gastroenteritis because the results do not alter clinical management, which mainly requires appropriate rehydration therapy.
Medical history and physical examination
The primary objective of obtaining a medical history and conducting a thorough physical examination is to assess whether an affected individual, who is most often a child, is dehydrated, but also to get some potential insights into the etiology of acute gastroenteritis. Thus, medical history should include the duration of illness, urination frequency, the nature of stools, the type of emesis, the presence of fever, and the assessment of mental status.
Three principal examination signs for determining dehydration in children include an abnormal skin turgor, abnormal respiratory pattern, and prolonged capillary refill time. Different scales are used to assess dehydration, the most common of which is that which is provided by the United States Centers for Disease Control and Prevention (CDC). Parental report of the child's symptoms can also aid significantly.
Serum electrolyte measurement is usually not required in children with mild to moderate dehydration. The child’s weight during the illness in comparison with the weight after treatment is used to retrospectively determine the degree of dehydration. Urine specific gravity and blood urea nitrogen measurements are poor markers of dehydration.
Laboratory diagnosis
Laboratory diagnosis of rotaviral infections is primarily achieved via enzyme immunoassays that involve detection of VP6 group A-specific antigen in diarrheal stools. As an alternative, the immunological detection of this antigen can be achieved through the capture of antigen from feces by anti-VP6-specific antibodies immobilized onto latex, nitrocellulose or nylon.
Although the commercial enzyme immunoassays that are used for rotavirus surveillance are sensitive and specific, regular quality control procedures are required in order to ensure that different laboratories are performing the commercial assay at high proficiency.
Electron microscopy is highly specific for the detection of rotavirus with sensitivity comparable to enzyme immunoassays. However, this method is labor-intensive and cumbersome for routine detection of rotavirus in large numbers of stool specimens. Furthermore, expensive instrumentation and highly trained personnel are needed for optimal results.
Rotaviral double-stranded RNA segments can be detected in clinical specimens via extraction of the viral RNA and subsequent analysis by electrophoresis on a polyacrylamide gel followed by silver staining. Silver ions form a stable complex with nucleic acids, thereby supporting the use of silver staining for this purpose.
Human rotavirus exhibits well-defined patterns of gene-segment distribution, which are also known as electropherotypes. The results of electropherotyping correlate with the presence of viruses of a specific group, as shown by using other methods. Consequently, the presence of distinct electropherotype patterns has long been considered diagnostic for the presence of individual rotaviruses.
A plethora of sensitive conventional or real-time reverse-transcription polymerase chain reaction (RT-PCR) methods have been developed based on the primers that are specific for different rotavirus genes. These methods have been exceptionally useful in detecting rotavirus in extraintestinal tissues, as well as for studying the correlation that exists between disease severity, virus load, and the duration of viral shedding in stool.
References
- https://www.icmr.gov.in/
- http://www.aafp.org/afp/2012/0601/p1059.html
- https://www.who.int/
- http://www.nlm.nih.gov/medlineplus/ency/article/003349.htm
- https://www.kliinikum.ee/infektsioonikontrolliteenistus/index.php
- http://library.ndsu.edu/tools/dspace/load/?file=/repository/bitstream/handle/10365/4395/farm_38_4_7.pdf?sequence=1
- Vaishnavi C. Infections of the Gastrointestinal System. JP Medical Ltd, 2013; pp. 321-329.
Further Reading
Last Updated: Feb 17, 2023