Skip to:
Physical exercise provides benefits that range from weight control and disease management to improved psychological wellbeing. Despite the many positive outcomes of physical exercise, community perception and lay press represent exercise as harmful to the joints, especially in the lower extremity.
What is osteoarthritis?
Osteoarthritis is a condition characterized by a structural and functional failure of synovial joints with loss and degradation of articulate cartilage, meniscal degeneration, and synovial inflammatory responses.
Synovial joints are located between bones that move against each other during movement, as with the joints of the limbs. The joint failure causes pain and disability.
The main symptoms of osteoarthritis are stiffness and joint pain. Some people also experience symptoms such as swelling and tenderness during movement.
Joints are constantly exposed to low-level damage. However, the body repairs itself and movement does not cause the above-mentioned symptoms. In the case of osteoarthritis, the protective cartilage of the joints breaks down leading to the pain during movement execution.
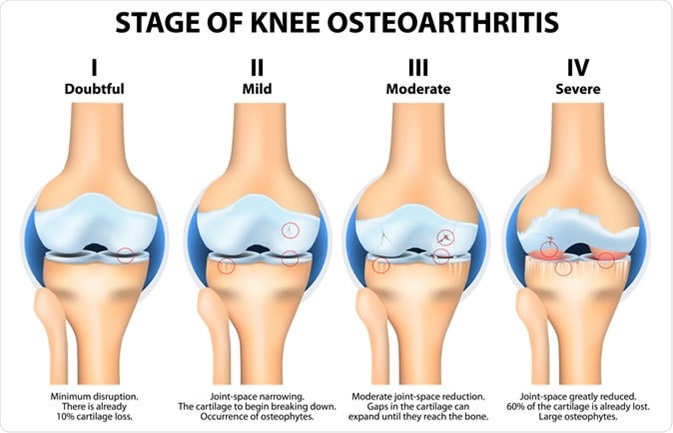
Stages of knee osteoarthritis (OA). Image Credit: Designua / Shutterstock
How is exercise beneficial for people with osteoarthritis?
Exercise is a central component of the management of osteoarthritis. Physical exercise is prescribed as a way to facilitate weight loss to reduce joint stress, improve functional performance by preserving joint range of motion, and reduce symptoms.
It is recommended that people with osteoarthritis take part in low- impact aerobic exercises such as swimming, cycling and other aquatic activities.
Aquatic exercise is preferred to land-based physical activity because the body buoyancy decreases the compressive load that the knees experience during movement.

Image Credit: pio3 / Shutterstock
Cycling is also beneficial for the same purpose as it partially unloads the knees and keeps them stable whilst providing a large range of motion.
Quadriceps weakness is a common symptom of osteoarthritis. However, studies have shown that quadriceps weakness can be present in people who do not have osteoarthritis. Hence, quadriceps weakness is considered a risk factor for the development of osteoarthritis because it leads to a decreased stability of the knee joint and it reduces the capacity of the muscles to attenuate shock.
A systematic review, focusing on the role of exercise therapy, has concluded that there is sufficient evidence regarding the advantages of exercise therapy in the treatment of patients with osteoarthritis. An exercise that strengthens the quadriceps leads to improvements in function and reduction of pain during movement.
Researchers recommend that strengthening exercise programs should start with isometric exercises and gradually incorporate isotonic resistance exercises when appropriate.
Isometric exercises are contractions of a muscle during which the muscle does not change in length and the affected joint does not move.
In contrast, in isotonic exercises the muscle contracts and it shortens against a constant load.
Recommended exercises
Physical exercise is considered the most effective non-drug method of reducing pain in patients with osteoarthritis. There is a range of different exercises recommended for improving the function and structure of joints.
Range of motion and flexibility exercise: These exercises require the investment of a full range of motion that joints are capable of. These include gentle stretching and movements that require the full span of joints.
Aerobic/endurance exercises: These include walking, jogging, swimming and cycling. This type of exercise reduces fatigue and builds stamina.
Aquatic exercises: These exercises help relieve the pressure of the joints whilst providing resistance to the muscles and strengthening them. Aquatic exercises help reduce pain and improve the daily function of people with osteoarthritis.
Adherence is the predictor of long-term outcomes of exercises in the knee or hip osteoarthritis. Thus, strategies that improve adherence should be adopted.
One of these strategies is long-term monitoring. In addition to that, long-term participation in physical activity requires patients to enjoy the exercises as this increases their motivation for participation.
High-velocity impact exercises such as running and step aerobics can be deleterious over the long-term in patients with osteoarthritis, so these types of exercises are not recommended.
Concluding remarks
Based on current evidence, people should be actively encouraged to exercise regardless of whether they have joint disease, as the benefits of exercise are numerous for joint health and other body systems.
Research shows that low-impact exercise does not lead to the development of osteoarthritis. On the contrary, strengthening muscles and engaging joints through their range of motion can help mitigate against joint damage.
People who take part in elite sports activities, susceptible to joint injury, are at a higher risk of developing osteoarthritis due to the rigorous exercises that they practice but it is not clear if high-impact exercise in the absence of injury or predisposition to osteoarthritis is harmful.
If an individual has a predisposition to developing osteoarthritis, it is vital to take into consideration the type of sports activity, the intensity of the activity, and the extent of the joint impact, body weight, and family history of osteoarthritis.
Taking into account all the benefits that physical exercise has, it will continue to play a crucial part in both the pathogenesis and management of osteoarthritis.
References
Further Reading
Last Updated: Oct 20, 2019