How does AMR affect STDs?
Global impact: The threat of drug-resistant STDs
Causes of antimicrobial resistance in STDs
Current challenges in treating antibiotic-resistant STDs
What can be done to combat antimicrobial resistance in STDs?
Conclusion
References
Further reading
Antimicrobial resistance (AMR) is among the top ten public health threats, causing 1.3 million deaths in 2019 – more than either AIDS or malaria – and contributes to 5,41,000 more.1,2
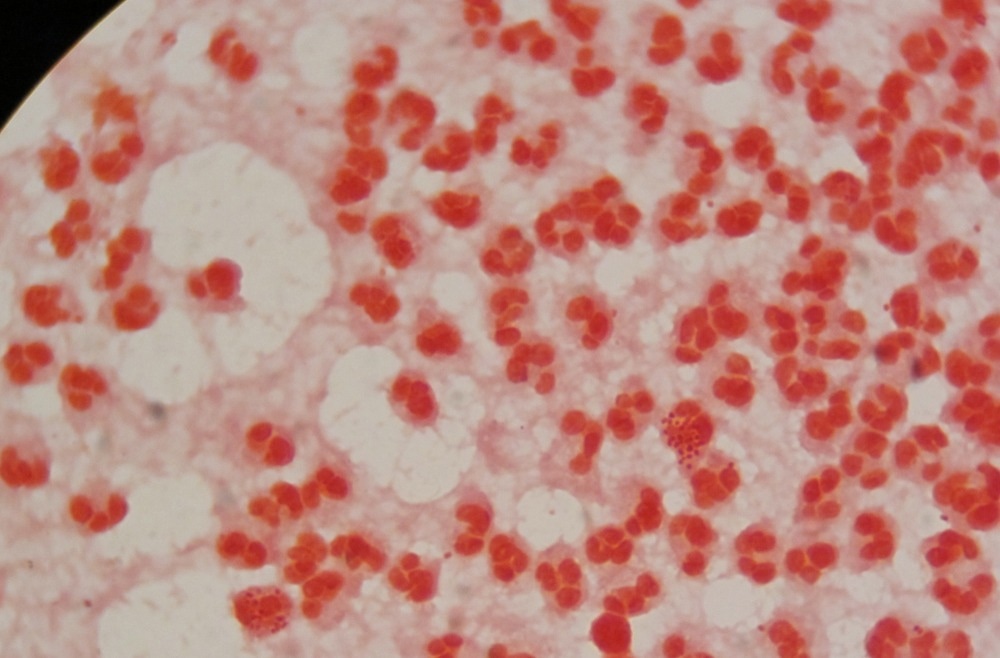
Image Credit: Sureerat niukoonchitt/Shutterstock.com
AMR can be transferred between organisms and species. In addition, resistant microbes themselves spread within and between plants, animals, and humans. They contaminate water, soil, and air, and they find wild reservoir hosts. AMR causes huge economic losses, increased healthcare costs, and reduced productivity and food security.2
How does AMR affect STDs?
According to the World Health Organization (WHO) there are 500 million new cases of sexually transmitted diseases (STDs) each year, with about 106 million each of chlamydial and gonorrheal infections and 10.6 million cases of syphilis.
These are caused by Chlamydia trachomatis, Neisseria gonorrhoeae, and Treponema pallidum, respectively. Mycoplasma genitalium is another common STD. pathogen. These result in infertility, miscarriage, stillbirth, and neonatal death, depending on the pathogen and the time of infection.4
The greatest concern among STDs is the rise of multi-drug resistant (MDR) N. gonorrheae strains. This microbe rapidly acquires and accumulates AMR mutations.4,5
Image Credit: Anastasiia Usenko/Shutterstock.com
“There are now strains of N. gonorrhoeae that are resistant to all major drugs used to treat gonorrhea, including β-lactams, fluoroquinolones, macrolides, tetracyclines, spectinomycin, cephalosporins, and azithromycin.”4
M. genitalium is also increasingly becoming treatment-resistant, with up to 51% of strains showing resistance to azithromycin in 2016, up from 10% before 2010.9
Some of these can spread rapidly (“high-risk clones”), while others acquire resistance to all or almost all drugs developed to treat them (“extensively drug-resistant” (XDR) or “pandrug resistant” strains, respectively).4
Global impact: The threat of drug-resistant STDs
AMR in STDs will enormously increase the global impact. It will be impossible to meet Global Health Sector Strategies that seek to reduce gonorrhea incidence by 90% by 2030 among people between 15 and 49 years unless AMR is addressed.10
For example, gonorrhea increases HIV transmission fivefold, causing infertility, neonatal blindness, pelvic inflammatory disease, ectopic pregnancy increased maternal mortality, and miscarriage.11
Treatment failures using last-resort drugs for gonorrhea have been reported in over ten high-income countries, which represent the minority of gonorrhea cases. “This suggests that reports of treatment failures and drug resistance in wealthier areas are only the tip of the global health burden.”11
Shortages of antibiotics used for STDs are reported or predicted, such as for benzathine penicillin for syphilis in pregnancy and first-line antibiotics used for chlamydia and trichomoniasis.6
Causes of antimicrobial resistance in STDs
AMR in STDs arises from factors such as the unrestricted availability of antimicrobials in several countries with a high STD burden, the routine overuse and misuse of antibiotics all over the world, poor antibiotic quality, and incomplete antibiotic treatment.11
Extra-genital asymptomatic infections of the pharynx and rectum, mostly in men who have sex with men, allow gonorrhea strains to acquire AMR genetic material from other organisms. These are often fast-spreading strains.11
Current challenges in treating antibiotic-resistant STDs
STDs increase the risk of acquiring HIV, which in turn increases the risk of STDs as well as opportunistic infections.6 With limited treatment and prophylactic options for many STDs, the future is challenging. New guidelines have been introduced for the treatment of several STDs.11
Sexually transmitted infections (STIs): Global Youth united to end antimicrobial resistance (AMR)
What can be done to combat antimicrobial resistance in STDs?
A multipronged strategy is essential to fight AMR in STDs. Psychosocial and behavioral interventions should back up public health education to increase awareness of this crisis.8
“Comprehensive sexual education, also referred to as “abstinence plus” or “sexual risk reduction,” promotes abstinence as the primary approach to prevent STIs but also encourages available barrier and contraceptive methods.” With strong evidence of utility, these should be scaled up and applied widely.8
Broad and effective regulation of hygiene and sanitation measures and antimicrobial sale and distribution are essential to minimize the threat of AMR. Adequate diagnosis with sensitive, reliable, and rapid molecular tests to detect the primary and opportunistic pathogens, with susceptibility testing, is key to appropriate treatment.4,5,7
Regional surveillance programs, such as the WHO Global Gonococcal Antimicrobial Surveillance Programme (WHO Global GASP), must monitor drug- and strain-specific resistance patterns.4,5 Reporting of treatment failures, along with investment in new laboratories and diagnostic methods, research into drug action and resistance mechanisms, and novel antibiotic development, are other key aspects of the required action plan.4,5,7
Conclusion
Prevention is better than cure. Public health preventive interventions, including psychosocial and behavioral interventions, must be prioritized. Broad regulatory diagnostic, prescribing, and reporting guidelines must be enforced.
All stakeholders, from the government to pharmaceutical companies, regulatory bodies, scientists, and healthcare professionals, as well as the public, should work together to avert this looming disaster.
References
- Estany-Gestal, A., Salgado-Barreira, A., and Varquez-Lago, J. M. (2024). Antibiotic Use and Antimicrobial Resistance: A Global Public Health Crisis. Antibiotics. doi: https://doi.org/10.3390%2Fantibiotics13090900. Available at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC11428428/. Accessed on October 7, 2024.
- Morier, D. (2024). Antibiotic resistance. Britannica Encyclopedia. Available at https://www.britannica.com/science/antibiotic-resistance. Accessed on October 7, 2024.
- What is antimicrobial resistance and why is it a growing threat? (2023). Retrieved from https://www.unep.org/news-and-stories/story/what-antimicrobial-resistance-and-why-it-growing-threat. Accessed on October 7, 2024.
- Shaskolskiy, B., Dementieva, E., Leinsoo, A., et al. (2016). Drug Resistance Mechanisms in Bacteria Causing Sexually Transmitted Diseases and Associated with Vaginosis. Frontiers in Microbiology. doi: https://doi.org/10.3389%2Ffmicb.2016.00747. Available at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4870398/. Accessed on October 7, 2024.
- Sena, A. C., Bachman, L., Johnston, C., et al. (2020). Optimising treatments for sexually transmitted infections: surveillance, pharmacokinetics and pharmacodynamics, therapeutic strategies, and molecular resistance prediction. Lancet Infectious Diseases. doi: https://doi.org/10.1016%2FS1473-3099(20)30171-7. Available at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8041119/. Accessed on October 7, 2024.
- De Vries, H. J. C. (2019). Current challenges in the clinical management of sexually transmitted infections. Journal of the International AIDS Society. doi: https://doi.org/10.1002%2Fjia2.25347. Available at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6715942/. Accessed on October 7, 2024.
- Ndowa, F., Lusti-Narasimhan, M., and Unemo, M. (2012). The serious threat of multidrug-resistant and untreatable gonorrhoea: the pressing need for global action to control the spread of antimicrobial resistance, and mitigate the impact on sexual and reproductive health. BMJ. doi: https://doi.org/10.1136/sextrans-2012-050674. Available at https://sti.bmj.com/content/88/5/317.long. Accessed on October 7, 2024.
- National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Population Health and Public Health Practice; Committee on Prevention and Control of Sexually Transmitted Infections in the United States; Crowley, J. S., Geller, A. B., Vermund, S. H. (eds.). Sexually Transmitted Infections: Adopting a Sexual Health Paradigm. Washington (DC): National Academies Press (US); 2021 Mar 24. 8, Psychosocial and Behavioral Interventions. Available at: https://www.ncbi.nlm.nih.gov/books/NBK573151/.
- Broom, A., Peterie, M., Ridge, D., et al. (2023). Sex, drugs and superbugs: The rise of drug resistant STIs. SSM – Qualitative Research in Health. doi: https://doi.org/10.1016/j.ssmqr.2023.100310. Available at https://www.sciencedirect.com/science/article/pii/S266732152300094X. Accessed on October 7, 2024.
- Addressing antimicrobial resistance in STIs. (2024). Retrieved from https://www.who.int/teams/global-hiv-hepatitis-and-stis-programmes/stis/treatment/addressing-amr-in-stis. Accessed on October 8, 2024.
- Multi-drug resistant gonorrhoea (2024). Retrieved from https://www.who.int/news-room/fact-sheets/detail/multi-drug-resistant-gonorrhoea. Accessed on October 8, 2024.
Further Reading
Last Updated: Oct 21, 2024