The symptoms and causes of andropause
Testosterone levels and male menopause
LOH diagnosis and treatment
How to debunk the myths of andropause
References
Further reading
Andropause is a natural age-related decline in testosterone and growth hormone levels in men. Several terminologies have been used to refer to andropause, including male menopause, male climacteric, androgen deficiency in aging males (ADAM), viropause, and partial androgen deficiency in aging males (PADAM).

Image Credit: Minerva Studio/Shutterstock.com
The World Congress on the Aging Male in Prague (2004) and the World Health Organisation in Paris (2003) described male menopause in two definitive terms, namely, late-onset hypogonadism (LOH) and the Aging Male Syndrome (AMS).
This article is focused on highlighting the main cause, symptoms, and treatment of this male dysfunction.
The symptoms and causes of andropause
The word "andropause" has been derived from the Greek word "andras" meaning human male, and "pause" means a cessation. Therefore, andropause refers to a condition where men experience a decrease in sexual satisfaction or a decline in overall well-being due to low testosterone levels in older men.
In 1946, the andropause syndrome was first described as "male climacteric," which was characterized by decreased libido, nervousness, irritability, erectile dysfunction, reduced potency, fatigue, reduced muscle mass and strength, hair loss, hot flushes, memory problems, depression, and sleep disturbances.
Hypogonadism is the main cause of the clinical symptoms of andropause. In contrast to menopause, a well-characterized and timely process linked to absolute gonadal failure, andropause is a more subtle androgen deficiency with slow progression. LOH, or functional hypogonadism, is characterized by a low blood testosterone concentration.
Besides old age, andropause also exists in men who lose their testicular function due to diseases or accidents. This syndrome has also been observed in men with advanced prostate cancer who undergo surgical or medical castration.
Testosterone levels and male menopause
Testosterone is the main androgen hormone responsible for key male sex characteristics. Hence, alteration in testosterone levels affects the psychological and sexual functions and body composition of the male population. The Massachusetts Male Aging Study (MMAS) and the New Mexico Aging Study revealed that inadequate testosterone levels in older men and other anabolic hormones increase mortality risk.
Testosterone levels decrease at the rate of 1% per year with aging. It must be noted that the rate of testosterone decline varies with people depending on multiple factors, including serious emotional stress, chronic disease, medications, and obesity. The decline rate can be effectively decelerated by managing health and lifestyle factors.
In aging men, the decline in testosterone levels is mainly due to a reduction in Leydig cell mass in the testicles, a dysfunction in the hypothalamic-pituitary homeostatic control, or both. These conditions lead to low secretion of luteinizing hormones and subsequent low testosterone production.
Although the decline in testosterone levels in males occurs gradually, it is most prominent between 40 and 55 years. It is imperative to address the adverse health effects linked to andropause to protect the aging male population from major health issues, including disabilities and morbidity.
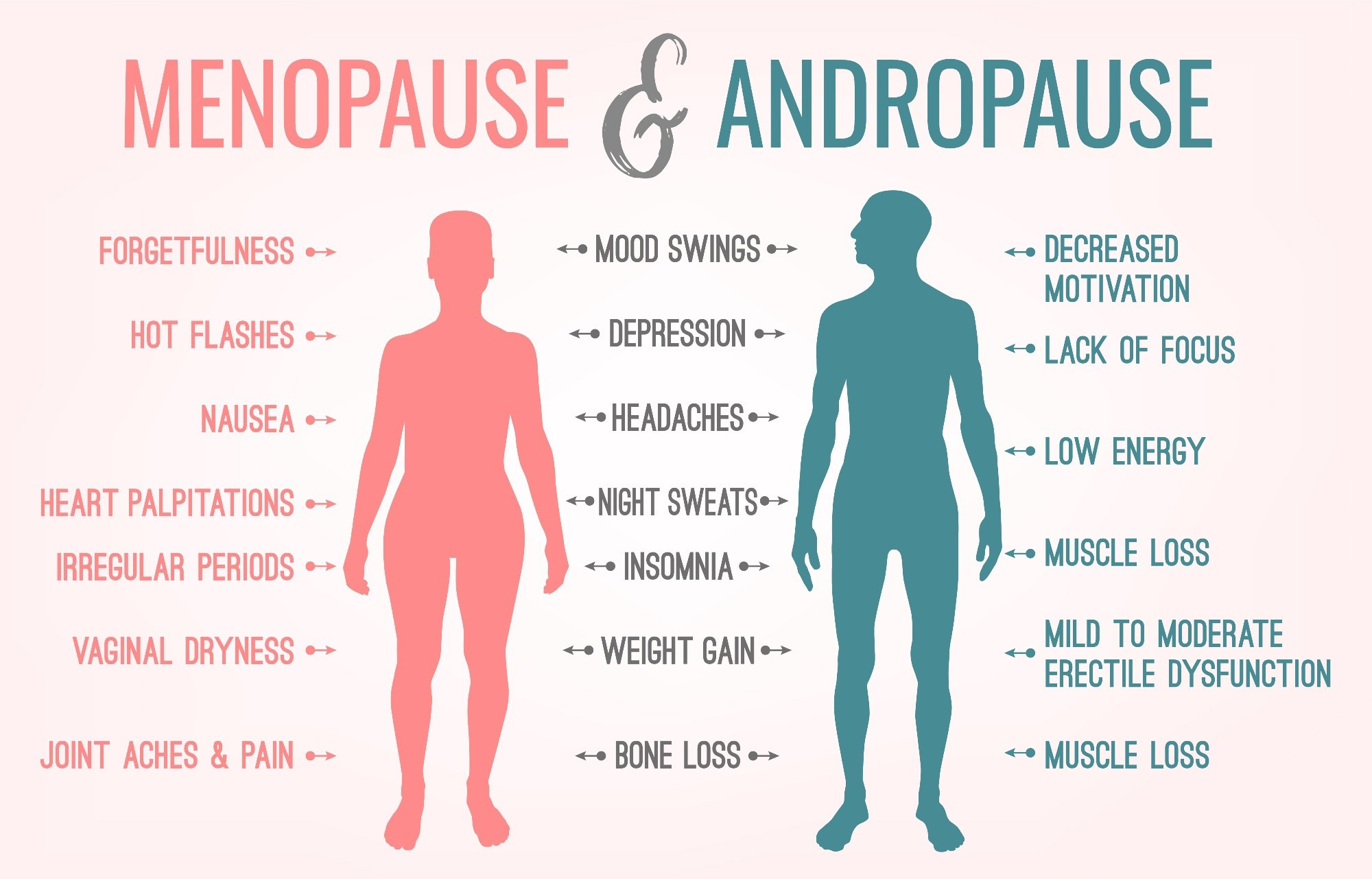
Image Credit: Double Brain/Shutterstock.com
LOH diagnosis and treatment
Diagnosing and treating LOH is important because it increases the risk of many chronic illnesses, including inflammatory arthritic disease, diabetes mellitus, renal disease, chronic obstructive lung disease, obesity, hemochromatosis, and human immunodeficiency virus (HIV)-related disease.
LOH is diagnosed based on clinical symptoms that indicate testosterone deficiency. One of the key clinical features of hypogonadism is low libido. As stated above, other manifestations include decreased bone mineral density, osteoporosis, increased body fat, decreased muscle mass and strength, erectile dysfunction, and depression. However, none of these symptoms are specific indicators of this condition. Clinicians mostly evaluate serum testosterone levels in the presence of more than one symptom.
Before LOH diagnosis, patients must not be prescribed antidepressants, digoxin, corticosteroids, opioid analgesics, antifungal agents, and spironolactone for symptomatic treatment, as these medications could hamper LOH diagnosis.
A total testosterone level of less than 11 nmol/l and a free testosterone level of less than 220 pmol/l is recommended as the minimum criteria for LOH diagnosis for the aging male population. Sulfate precipitation and equilibrium dialysis are the gold standards used to estimate free testosterone and bioavailable testosterone.
Patients with critically low testosterone levels are treated with testosterone replacement therapy. This therapy has improved body composition, decreased fat mass, and increased muscle mass and strength. In addition, this treatment enhanced bone density in hypogonadal men of all ages.
Testosterone therapy improves serum testosterone levels, significantly enhancing libido and alleviating erectile and orgasmic function. This treatment also positively reduced the risk factors for cardiovascular events and metabolic syndrome, such as obesity, hypertension, impaired insulin resistance, and dyslipidemia.
Androgens stimulate erythropoiesis and improve bone marrow erythropoietic activity, reticulocyte count, and hemoglobin. Therefore, androgen therapy is extremely useful in treating people with anemia. Since reduced testosterone level affects visuospatial performance and verbal and visual memory, it could be assumed that this therapy would improve multiple cognitive functions.
How to debunk the myths of andropause
Many men are misinformed about the clinical conditions of andropause and suffer from significant dilemmas regarding this condition. It is important to address male menopause with proper information.
Male Menopause Explained
The lack of awareness, improper understanding, ignorance, and unquestionable acceptance of male menopause are the root causes of the myths associated with its manifestations. Many men who visit general physicians due to fatigue and lack of libido are sent back saying, "It's your age', without addressing the possibility of male menopause onset. Furthermore, many individuals with andropause are misdiagnosed with depression and are prescribed anti-depressants.
There is a need to increase awareness regarding andropause through the education system. Increased awareness about testosterone replacement therapy to alleviate andropause conditions could benefit many males in the rapidly aging global population.
References
- Mohammadi, M. et al. (2023) The Prevalence of Andropause and Its Relationship With Sexual Quality of Life Among Older Iranian Men. American Journal of Men's Health. https://doi.org/10.1177/15579883231161050
- Mian, A. H. et al. (2022) Current Management and Controversies Surrounding Andropause. Urologic Clinics of North America, 49(4), pp. 583-592. https://doi.org/10.1016/j.ucl.2022.07.003
- Martelli, M. et al. (2021) Influence of Work on Andropause and Menopause: A Systematic Review. International Journal of Environmental Research and Public Health, 18(19). https://doi.org/10.3390/ijerph181910074
- Mousavi, M. et al. (2018) Exploratory Study of Andropause Syndrome in 40-65 Years in Arak: A Cross Sectional Study. Journal of Family & Reproductive Health, 12(3), pp.142-147. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6571447/
- Singh, P. (2013). Andropause: Current concepts. Indian Journal of Endocrinology and Metabolism, 17(13), pp.S621. https://doi.org/10.4103/2230-8210.123552
- Wespes, E. and Schulman, C. C. (2002) Male andropause: Myth, reality, and treatment. International Journal of Impotence Research, 14(1), pp. S93-S98. https://doi.org/10.1038/sj.ijir.3900798
Further Reading
Last Updated: Oct 25, 2023