The thymus unveiled: understanding its anatomy
The crucial function of the thymus
Maturation in the thymic microenvironment
Thymus and immune disorders
Changes over a lifetime
Conclusion
References
Further reading
An essential component of the lymphatic system, the thymus, a pyramid-shaped organ located in the thoracic cavity, is responsible for producing T-cells. For centuries, the thymus was believed to be an enigmatic organ, and there was no accurate description of its functions. Research over the years has provided insight into this organ's structure and various functions. As essential components of an effective adaptive immune system, the thymus develops responsive T-cells from immature progenitors.

Image Credit: Magic mine/Shutterstock.com
The thymus unveiled: understanding its anatomy
It is a lymphoid organ made of two lobes situated behind the sternum, between the lungs. Mainly composed of epithelial cells, lymphocytes, and dendritic cells, the thymus comprises two parts – medulla and cortex. The epithelial cells, known as TECs (thymic epithelial cells), are further classified into cTECs (cortical TECs) and mTECs (medulla TECs). Thymic organogenesis is governed by the highly potent Tecs produced during early fetal development.
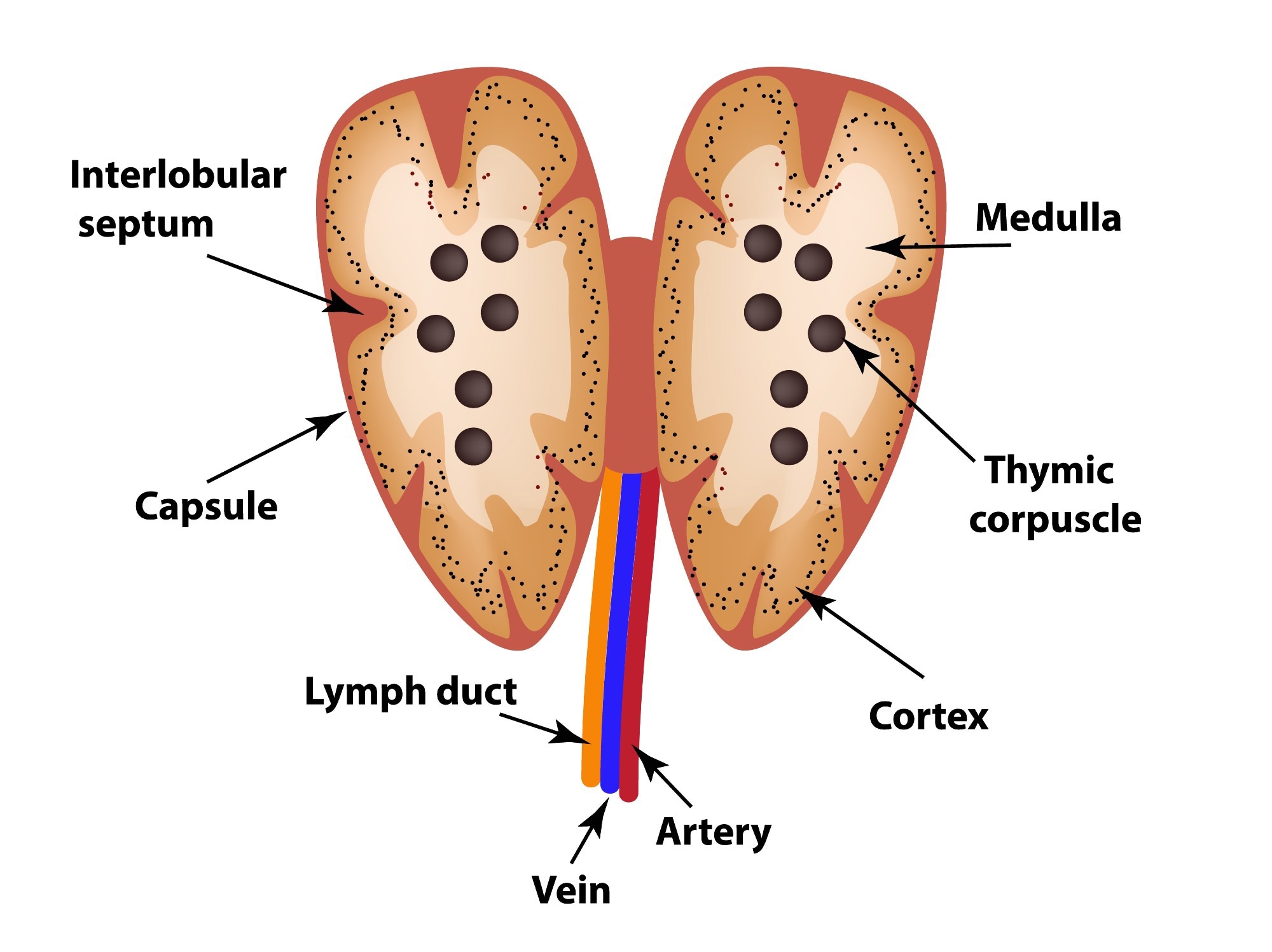 Structure of the thymus. Image Credit: Sakurra / Shutterstock
Structure of the thymus. Image Credit: Sakurra / Shutterstock
The crucial function of the thymus
The thymus is a critical organ of the immune system and helps the body fight against several foreign bodies, including pathogens and antigens. The thymus aids in generating T-cells, which are involved in fighting infections. T-cells are produced via multiple stages of differentiation and proliferation.
It is primarily involved in developing mature T-cells by promoting the differentiation of bone-marrow-derived lymphocyte progenitors. T-cells play a role in various aspects of tissue physiology and pathology, including tissue healing, eclampsia, dysbiosis, and cancer.
The thymus is also vital for the central self-tolerance mechanism, which focuses on clonal deletion of the self-reactive T-cells. The cTECs are responsible for a process of positive selection. In this mechanism, only those T-cells survive who do not react with the self-antigens. The mTECs are involved in the negative selection of lymphocytes, which are eliminated through apoptosis.
Maturation in the thymic microenvironment
The appropriate maturation of thymocytes into functionally capable, self-tolerant T-cells and the eradication of autoreactive T-cells depend on a normal thymic microenvironment.
The fetal and postnatal formation and maintenance of all TEC depend on the transcription factor FoxN1. Human autoimmune illness and loss of thymic structure are caused by FoxN1 deficiency. AIRE protein, a crucial transcription factor for TEC function, is exclusively produced by mTECs and promotes promiscuous expression of tissue-restricted antigens (TRAs), including kidney- and pancreas-specific proteins like insulin.
By interacting with P-selectin on thymic endothelial cells, lymphoid progenitors expressing platelet (P)-selected glycoprotein ligand 1 (PSGL1) circulate out of the bone marrow and enter the thymus. Their movement guides the appropriate development of thymocytes within the thymic microenvironment.
The crucial thymic functions (positive and negative selections) ensure that T-cells can identify antigens in the presence of self-MHC (major histocompatibility complex) but do not trigger self-reactivity. The resulting naive T lymphocytes occupy numerous secondary lymphoid organs, such as the spleen and numerous lymph nodes.
The antigens provided by dendritic cells in lymphoid locations stimulate naive T-cells, causing them to proliferate and differentiate into effector cells that can go to various organs where pathogens are encountered. Various effector T-cell subtypes mediate various activities, such as inducing direct cellular cytotoxicity against virally infected cells and boosting inflammatory responses.
Image Credit: Design_Cells/Shutterstock.com
Thymus and immune disorders
Thymus malfunction causes significant disruptions in the body's immune system, and thymus hyperactivity causes major autoimmune and proliferative illnesses. The thymus is a sensitive organ that reacts negatively to stress, alcohol, and drugs, which can lead to hypertrophy.
Myasthenia gravis is an autoimmune condition that frequently coexists with thymus enlargement. Other autoimmune conditions, including hyperthyroidism or systemic lupus erythematosus, can also bring on thymic hyperplasia.
Congenital diseases, including Di George syndrome and severe combined immunodeficiency (SCID), can also cause thymus atrophy. Other potential neoplastic causes of thymic hyperplasia include lymphomas and thymomas.
Thymolipomas are soft, uncommon tumors that can affect any age group. They are malleable tumors with a fatty composition. At the time of diagnosis, 50% to 65% of patients had metastases, making them more aggressive than thymomas. Most thymic tumors contain varying amounts of lymphocytes and non-malignant-appearing thymic epithelial cells.
Thymomas, typically asymptomatic, are discovered as accidental findings on chest radiography. They are associated with several auto-immune conditions, including neuromuscular (myasthenia gravis), endocrine (grave's disease), hematological (agranulocytosis), gastrointestinal, and cutaneous disorders.
Many different pathways have explained the development of immunological problems due to thymic malignancies. These include the AIRE (autoimmune regulator) theory, the genetic theory, and the escape theory.
As long as thymic tumors are entirely removed, surgery is the cornerstone of therapy. The gold standard in pharmacotherapy is still cytotoxic chemotherapy. However, pembrolizumab, sunitinib, and lenvatinib have been created to treat thymic carcinomas. Sometimes, the thymus is removed, as in the case of patients who have thymomas.
Inside the Thymus
It may be possible for residual thymic function or thymic regeneration to restore the patient's defense. The thymus may occasionally be transplanted to build tolerance or establish immunity. This method has promise for modulating T-cell tolerance and ensuring immune system reconstitution following immunosuppressive therapies.
Numerous attempts have been made to revive thymus function using tissue-engineering methods to create artificial thymus organoids or grow thymus tissues in vivo. Reversal immunosenescence in the elderly and solid organ transplantation will be the areas where thymus engineering can be advantageous.
Thymus bioengineering is still in its early stages, and additional study is required to enhance the technology for therapeutic use. A promising strategy to control the patient's adaptive immunity, thymus bioengineering can aid in achieving tissue/organ replacement without immunosuppression.
Changes over a lifetime
The thymus is known to be larger during infancy and regresses in both size and cellularity as the person moves through puberty to old age. The thymus develops throughout pregnancy, and the organ reaches functional maturity during the postpartum period. After that, as people age, the thymus's functions gradually decline.
Adult thymuses are comparatively much smaller than those of children. The organ also starts to lose structure and accumulate more fat cells. Age-related decrease in the immune response results from this process called thymus involution.
Conclusion
The thymus offers a unique environment for growing incredibly diverse and useful T lymphocytes. Surprisingly, most functional and regulatory components of thymus-dependent T-cell responses originate in the first few years of life.
Targeting thymic regeneration and modifying thymic output can be therapeutic for enhancing the formation of fresh naive T-cells in vaccines and encouraging the restoration of human T-cells following treatments that severely deplete them.
Understanding thymus function has significantly advanced the understanding of immune cell interactions and altered the course of both immunology and medicine. It has emphasized the importance of an up-to-date review of immunological events, including autoimmunity, immunodeficiency, memory, tolerance, and inflammatory and immunopathological disease situations.
Additional research into the thymus's workings and the relationship between T-cells and autoimmune diseases may reveal new information that can assist in creating novel treatments.
References
- Muto, Y., & Okuma, Y. (2022). Therapeutic options in thymomas and thymic carcinomas. Expert review of anticancer therapy, 22(4), 401–413. https://doi.org/10.1080/14737140.2022.2052278
- Miller J. F. A. P. (2020). The function of the thymus and its impact on modern medicine. Science (New York, N.Y.), 369(6503), eaba2429. https://doi.org/10.1126/science.aba2429
- Thapa, P., & Farber, D. L. (2019). The Role of the Thymus in the Immune Response. Thoracic surgery clinics, 29(2), 123–131. https://doi.org/10.1016/j.thorsurg.2018.12.001
- Manchanda, S., Bhalla, A. S., Jana, M., & Gupta, A. K. (2017). Imaging of the pediatric thymus: Clinicoradiologic approach. World journal of clinical pediatrics, 6(1), 10–23. https://doi.org/10.5409/wjcp.v6.i1.10
- Zdrojewicz, Z., Pachura, E., & Pachura, P. (2016). The Thymus: A Forgotten, But Very Important Organ. Advances in clinical and experimental medicine : official organ Wroclaw Medical University, 25(2), 369–375. https://doi.org/10.17219/acem/58802
- Tajima, A., Pradhan, I., Trucco, M., & Fan, Y. (2016). Restoration of Thymus Function with Bioengineered Thymus Organoids. Current stem cell reports, 2(2), 128–139. https://doi.org/10.1007/s40778-016-0040-x
- Weksler, B., & Lu, B. (2014). Alterations of the immune system in thymic malignancies. Journal of thoracic oncology : official publication of the International Association for the Study of Lung Cancer, 9(9 Suppl 2), S137–S142. https://doi.org/10.1097/JTO.0000000000000299
Last Updated: Oct 11, 2023