When a patient is suspected to have vaginitis, it is essential that a correct diagnosis is made to ensure the optimal treatment is carried out. There are several different types of vaginitis and each is associated with a unique treatment; if the wrong diagnosis is made the vaginitis symptoms may worsen.
.jpg) Illustration of bacterial vaginosis. Image Credit: Kateryna Kon / Shutterstock.com
Illustration of bacterial vaginosis. Image Credit: Kateryna Kon / Shutterstock.com
Indicative Symptoms
Although the symptoms of vaginitis can vary greatly among women with the condition and some do not experience symptoms at all, there are some signs that are known to be indicative of vaginitis. These include:
- Abnormal discharge from the vagina
- Unpleasant odor from groin area
- Pain or burning, particularly upon urination
- Itching on the outside of the vagina
- Pain or discomfort during sexual intercourse
Normal and abnormal discharge
It is normal for a woman to produce a discharge from the vagina, which can vary in color and consistency throughout different stages of the menstrual cycle. It can range from thin and watery to thick and creamy in color.
The discharge is usually described as abnormal when it leads to irritation, with symptoms of itching or burning in the area. Depending on the cause of the inflammation, the characteristics of the discharge that may lead to symptoms can vary greatly.
Types of Vaginitis
Vaginitis is categorized according to the cause of the inflammation, which has a direct impact on the way it should be treated.
The most common types of vaginitis are:
- Candida infection: marked by a thick, white, odorless discharge and often occurs following a course of antibiotics or changes in hormonal levels.
- Bacterial infection: discharge varies according to causative bacteria by usually milky consistency with a distinctive fish-like smell.
- Chemical irritation: associated with an inflammatory response due to contact with an irritant substance and may not alter vaginal discharge.
- Chlamydia or gonorrhea infection: associated with abdominal pain and abnormal menstrual bleeding, particularly after sexual intercourse.
- Trichomoniasis infection: marked by a frothy, pungent discharge that is green-yellow in color and may cause itching and soreness in the area.
- Herpes simplex viral (HSV) infection: associated with lesions on the vulva or inside the vagina that cause significant pain.
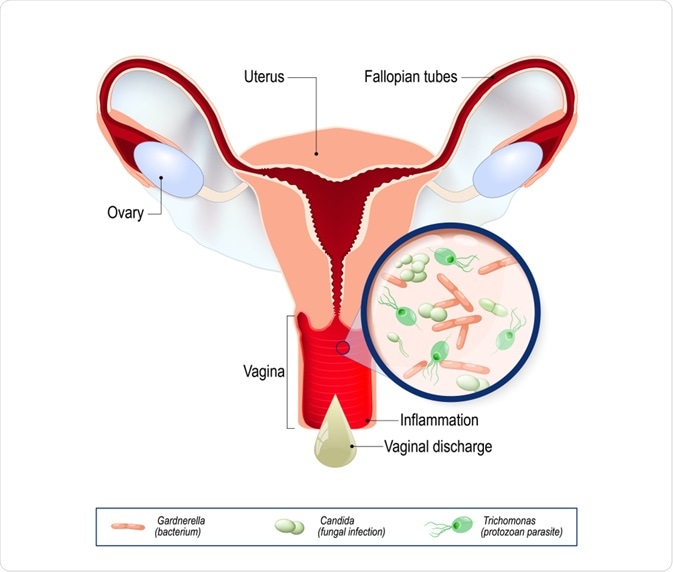 Vaginal infection and causative agents of vulvovaginitis. Image Credit: Designua / Shutterstock.com
Vaginal infection and causative agents of vulvovaginitis. Image Credit: Designua / Shutterstock.com
Differential diagnosis
Each of the different types of vaginitis described above require different management plans in order to lessen the inflammatory response in the vaginal area and related symptoms.
Initially, it is important to conduct a history of the symptoms, including their duration and severity. The nature of the discharge is a key point in reaching the true diagnosis. It is important to question the color, consistency, odor and quantity of the discharge. Other related symptoms that should be discussed are itchiness and pain, particularly those associated with sexual intercourse.
A physical examination is then undertaken and it is often necessary to take a swab from the vaginal area to be tested in a medical laboratory for causative organism. This is routinely practiced in regular pap smear exams to detect infections that may not be causing symptoms, such as chlamydia or gonorrhea, as well as on a case-by-case basis when a woman presents with symptoms.
In addition to the different types of vaginitis, symptoms can often be confused with women who have a urinary tract infection, leading to misdiagnosis. The distinctive points of difference lie in the vaginal discharge and pain on urination. Whereas a woman with vaginitis is likely to have unusual discharge, burning when urinating is the most common symptom associated with a urinary tract infection.
References
Further Reading
Last Updated: Feb 9, 2021