An amebicide is an agent used to treat patients with amebiasis. Amoebiasis is an infection that is caused by the amoeba, or unicellular organisms, of the Entamoeba genus. Antiamebic drugs or amebicides specifically target undestroyed amoeba.
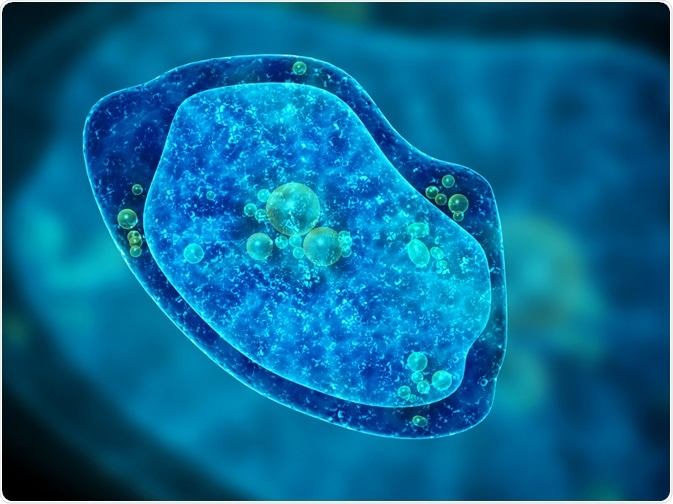 Image Credit: Lukiyanova Natalia frenta/Shutterstock.com
Image Credit: Lukiyanova Natalia frenta/Shutterstock.com
What is amebiasis?
Amebiasis is often asymptomatic but may cause dysentery and invasive extra-intestinal disease. It is caused by the ingestion of mature cysts in food or water, or on hands contaminated by feces. Once in the small intestine, the cysts of the Entamoeba release amoebic parasites (called trophozoites). Flask-shaped ulcers are formed following epithelial cell invasion in the large intestines.
The infection may spread (become systemic) from the site of infection in the intestines to other organs, to cause, for example, liver abscesses. Amebiasis is a predominant cause of severe diarrhea worldwide, and in the developing world, is among the top 15 causes of diarrhea in the first two years of life in children.
Amebiasis is the third cause of gastrointestinal diseases in returning international travelers, and it is also estimated that it accounts for 55,500 deaths in 2.2237 million disability-adjusted life years, which is defined as the total years of life lost and years lived with I disability, in 2010.
How are amebicides classified?
No vaccine against amebiasis exists at present, vassal treatment is via antiamebic drugs; these are prescribed depending on the severity of the infection and may be classified into three groups; this classification is based according to the site where the drug is effective.
Amebicides can be used to treat both mild and asymptomatic forms of amebiasis. Their use has contributed to reducing the morbidity and mortality of the disease:
- Systemic: effective against amoebas in the intestinal wall and liver (chloroquine, emetine, and dehydroemetine)
- Luminal: effective against amoebas present in the lumen of the intestine (paromomycin and iodoquinol)
- Mixed: effective against both lumina Lance systemic forms of amebiasis (metronidazole and tinidazole)
What are luminal amebicides?
Luminal amebicides act luminally (in the intestinal lumen) and encompass diiodohydroxyquinoline, diloxanide furoate, alongside iodoquinol and paromomycin. These luminal amebicides are active only against the intestinal forms of amoeba.
They are effective against the cyst and trophozoite forms of the ameba and are used in asymptomatic cyst carriers and intestinal amebiasis. As amebae feed on the intestinal flora, tetracycline is added to luminal amebicides to decrease major food sources.
What are mixed amebicides?
By contrast, the most used tissue and mixed amebicides all comprised of nitroimidazoles. Mixed amebicides are active against both intestinal and systemic forms of amebiasis. They include nitroimidazoles, which are a class of antibacterial that include metronidazole and tinidazole.
Nitroimidazoles work by inhibiting DNA synthesis. These agents are also considered to be bactericidal and indicated for the treatment of both gram-negative and gram-positive anaerobic bacterial infections, as well as protozoal infections such as intestinal and extraintestinal amebiasis.
Metronidazole is an example of a prodrug, which are inactive compounds created by modification of biologically active compounds and serve to increase drug permeation and drug delivery as the active constituent is released after the metabolism of the drug.
In the case of metronidazole, reduction by the parasites thioredoxin reductase and thioredoxin produces a nitroradical anion, which is further reduced, produces a nitroimidazole which targets the DNA of the amoeba, resulting in cell death. It is the drug of choice for amebiasis and is particularly effective against the anaerobic protozoa Giardia duodenalis, Trichomonas vaginalis, as well as Entamoeba.
Metronidazole is administered orally and rapidly absorbed, achieving peak plasma concentration between 1 and 3 hours of ingestion with a half-life of approximately 7 hours. It is distributed throughout the body tissues reaching high concentrations in body fluids which include the cerebrospinal fluid.
Metronidazole Is associated with several side effects which include vomiting, nausea, headaches, a metallic or bitter taste in the mouth, and more serious adverse events search as skin rashes coma anorexia, and ataxia (a group of disorders that affect balance, coordination, and speech).
Metronidazole may not be successful in eliminating amoebic cysts from the intestine; this, combined with its notable unpleasant adverse events, has led to the development of alternative drugs.
Tinidazole is a second-generation nitroimidazole that is similar to metronidazole in the spectrum of activity, absorption, adverse effects, and drug interactions. However, it has a simpler dosing regimen, less toxicity, and has a longer half-life, than metronidazole. A Cochrane review suggests that tinidazole may be better for reducing clinical symptoms and fewer adverse events when compared to metronidazole.
ANTIAMOEBIC || PHARMACOLOGY || Tissue and luminal Amoebicidal ||
What are systemic amebicides?
Systemic amebicides are used to treat amebic dysentery or hepatic abscesses. They are typically only effective in these severe cases and include dehydroemetine and chloroquine. Chloroquine eliminates trophozoites in liver abscesses, but it is not useful in treating luminal amebiasis; it is also effective in the treatment of malaria.
Dehydroemetine and emetine are derived from ipecac plant alkaloids and inhibit protein synthesis by blocking chain elongation. Adverse effects include pain at the site of injection, nausea, cardiotoxicity (arrhythmias and congestive heart failure), neuromuscular weakness, dizziness, and rash.
Overall, a Cochrane review of 41 trials (4999 participants) suggests that combination drug therapy may be more effective than metronidazole alone for eradicating ameba. Globally, amebiasis remains a public health burden and in developing countries despite advancements in control programs delivered by the WHO for neglected tropical diseases.
References
- Othman N, Ujang JA, Ng YL, et al (2020). Chapter 1 - Amebiasis In G Misra & V Srivastava (Eds), Molecular Advancements in Tropical Diseases Drug Discovery (pp.1–19). Academic Press.
- Nagaraja S, Ankri S (2019). Target identification and intervention strategies against amebiasis. Drug Resist Updat. doi.org/10.1016/j.drup.2019.04.003.
- Gonzales MLM, Dans LF, Sio-Aguilar J (2019). Antiamoebic drugs for treating amoebic colitis. Cochrane Database Syst Rev. doi.org/10.1002/14651858.CD006085.pub3.
- Shirley DT, Farr L, Watanabe K, et al (2018). A Review of the Global Burden, New Diagnostics, and Current Therapeutics for Amebiasis. Open Forum Infect Dis. doi.org/10.1093/ofid/ofy161.
- Kimura M, Nakamura T, Nawa Y (2007). Experience with intravenous metronidazole to treat moderate-to-severe amebiasis in Japan. Am J Trop Med Hyg. doi.org/10.1093/ofid/ofy161.
Further Reading
Last Updated: Sep 27, 2021