Over 700 bacterial species co-inhabit healthy human mouth. These species exist at diverse locations in the mouth including hard palate, soft palate, teeth, tongue, and even tonsillar area.
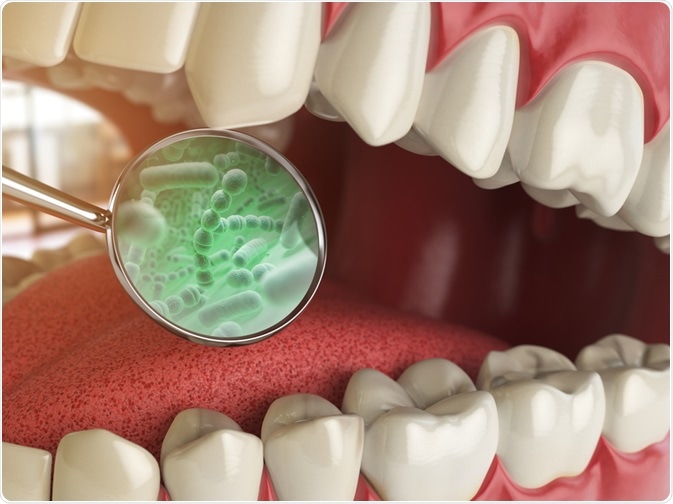
Image Credit: Maxx-Studio/Shutterstock.com
What are Commensals of the Oral Cavity?
Most of the microorganisms that inhabit the oral cavity live in a symbiotic relationship. Symbiosis means where both the host and guest coexist mutually for the benefit of each other. Commensals of the oral cavity keep a close watch on the growth of species which may pose harm to human health. They prevent the adherence of microorganisms which can stick to the mucosa or tooth surfaces.
Broadly these microorganisms belong to Streptococcus, Eubacteria, Fusobacterium, Capnocytophaga, Eubacteria, Staphylococcus, Eikenella, Porphyromona, Leptotrichia, Prevotella, Peptostreptococcus, Treponema, Actinomyces genera.
Some bacteria like Streptococcus, Granulicatella, Gemella, and Veillonella are amongst the predominant microorganisms of the oral cavity; however, the majority of bacteria are explicit to certain sites. Around 20 to 30 diverse species were found at a specific site and the ratio varies from 34 to 72 at different oral locations.
Understanding these oral floras can help in assessing various dental diseases like gingivitis and periodontitis which account for the most frequent bacterial infections in the human body.
More importantly, these microorganisms can even result in serious systemic infections like bacterial endocarditis, preterm labor, pneumonia, and cardiovascular diseases.
What is a dental biofilm and its adverse effect on dental health?
Dental biofilm is the first sign of forecasted dental problems. Microorganisms present in the oral cavity form a layer on the oral surfaces. Once a single layer is formed, these microorganisms start pilling up and form multiple layers which result in the formation of a multicellular matrix. Microscopic evaluation of these biofilms indicated that streptococcus accounts for approximately 80 percent of this colonization.
Soon after establishing multilayered biofilms streptococci establish adhesions on their surfaces. These adhesions are made of proteins and antigens. Besides streptococci, various other microorganisms can also form biofilms at varied sites.
The oral microbiome is susceptible to frequent disruptions caused by the host. Routine oral hygiene practices can disturb these biofilms. However, over some time these microorganisms do survive in the presence of various inhibitory actions like brushing, flossing, mastication of food, and swishing with oral disinfectants.
Which diseases are associated with oral microbiota?
Biofilms present in the oral cavity are essential for the sustenance of good oral health but an increase in the volume and complexities of these biofilms can result in diseases like gingivitis and Periodontitis.
Biofilms are primarily composed of Gram-positive anaerobic bacteria like Streptococcus anginosus and A.naeslundii; however, unhygienic conditions can dwell Gram-negative bacteria like Porphyromonas spp., Treponema denticola, Campylobacter spp, and A. actinomycetemcomitans.
Studies have highlighted that if dental hygiene is not maintained these Gram-negative bacteria can infect other organs. For example, bacterial endocarditis is one such condition that can affect the human heart. Besides this, bad breath, infection of the dental roots, and actinomycosis are also listed as some of the other concerns by these biofilms.
Maintaining good oral hygiene is the backbone of prevention of many diseases. Though not always but complex dental treatments can even transport these bacteria to the bloodstream, vital organs like lungs, kidneys, and brain.
Research has shown a close association between periodontal diseases and diseases of the respiratory system. Oral microbiota can act as a storehouse of various respiratory pathogens especially in patients admitted to intensive care units. Regular swishing with oral disinfectants like chlorhexidine and antiseptic solutions can ward off these bacteria.
Fungal infections in the oral cavity can be a result of the growth of fungal biofilms. C. Albicans are naturally occurring fungi in the oral cavity but in the presence of unhygienic conditions, it quickly multiplies and grows especially on the hard surfaces like dentures.
One recent research conducted at Harvard University has even indicated that one oral bacteria named P.gingivalis can cause serious health concerns like Alzheimer’s disease.
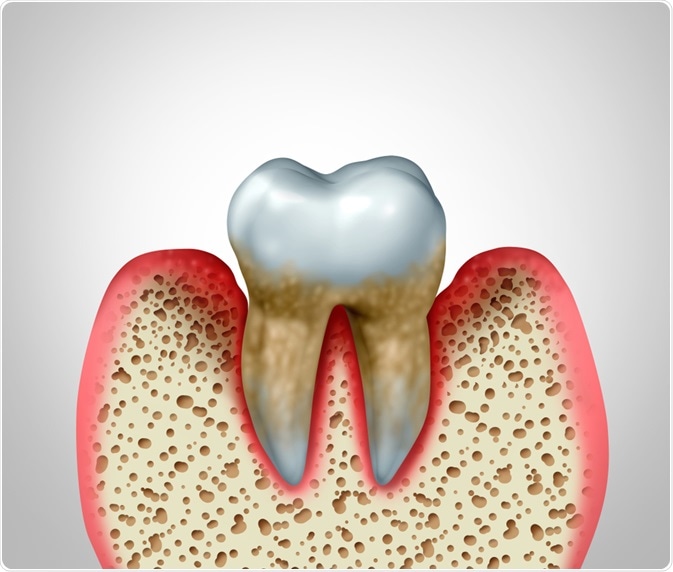
Image Credit: Lightspring/Shutterstock.com
Can probiotics help in reducing the overproduction of oral microorganisms?
Over the past few years, probiotics have shown great benefits in aiding good health, but less is known about the impact of intake of probiotics on oral health. Due to the emergence of antibiotic-resistant bacteria, probiotic-based dental products are becoming popular.
One such study was conducted to assess the effect of probiotics on oral health. The results revealed that probiotics can help in neutralizing the highly acidic environment of the oral cavity and thereby, prevents the activity of cariogenic bacteria.
Results also reflected that patients suffering from dental concerns like gingivitis and periodontitis showed marked improvement in their gum health post chewing probiotic-based chewing gums. Swishing the mouth with probiotic-based mouthwashes prevented the growth of sulfur-based bacteria resulting in an odor-free breath.
Further Reading
Last Updated: Sep 16, 2020