Using similar technology to 3D printing, bioprinting uses a digital file as a blueprint to fabricate biomedical parts that closely imitate the characteristics of natural tissue. The engineered tissues are created by layering biomaterials and/or living cells, which are referred to collectively as bio-inks.
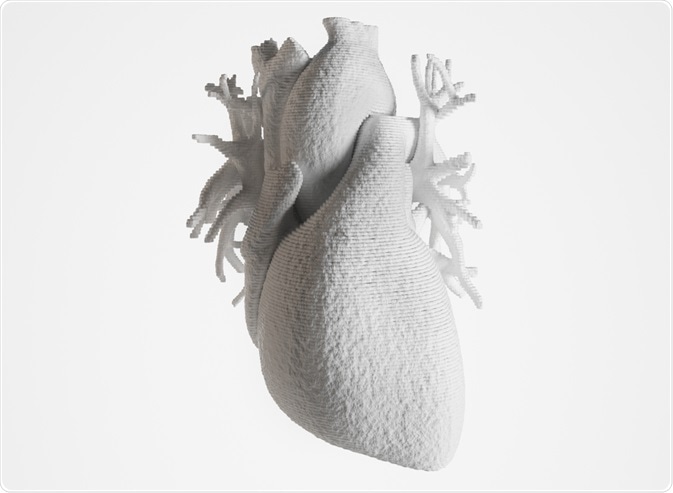 Image Credit: Crevis / Shutterstock.com
Image Credit: Crevis / Shutterstock.com
Bio-inks must possess certain physicochemical properties to ensure that the resultant tissue constructs are adequately robust, biologically compatible with the tissues they mimic, and able to be produced at scale.
Bioprinting occurs in three stages:
Pre-bioprinting
This involves the production of the digital model that will later be printed and the selection of the materials that will be used. Images are usually created with computerized tomography or magnetic resonance imaging and once finalized, certain cells are isolated, multiplied and combined with the selected bio-ink.
Bioprinting
The cell-laded bio-ink is placed into a cartridge and the necessary printheads for creating the target structure are selected.
Post-bioprinting
This stage is necessary to ensure the stability of the printed structure and involves providing it with mechanical and chemical stimulation to control cell growth.
Although bioprinting is a relatively new technology, its potential applications are far-reaching and revolutionary. In research, bio-printed tissue provides a cost-effective and regulation-free option for early drug safety and efficacy testing and has been used to investigate cancer pathology and growth. Clinically, bioprinting offers the potential to generate personalized organs for transplant in the laboratory.
Why bioprint organs?
The demand for organ transplantation has rapidly grown over the past two decades. Worldwide increases in the incidence of end-stage organ failure combined with rising successes in post-transplantation outcomes has resulted in an organ shortage crisis, as the demand for organs vastly outstrips supply.
Although many countries have national donation programs including both explicit and presumed consent processes, waiting lists for organs remain long. Post-operatively, the immune system of the transplant recipient may recognize the new organ as ‘foreign’ and trigger transplant rejection.
The potential to eliminate the reliance on donated organs for transplant, whilst simultaneously reducing the risk of transplant rejection by using bio-inks would, therefore, be ground-breaking.
Recent developments in organ bioprinting
Currently, the ability to bioprint functional organs remains elusive, with the integration with the vascular network proving the most problematic challenge. Without vascularization, the printed organ is unable to perform the functions necessary for maturation such as obtaining nutrients and waste removal, ultimately leading to organ malfunction.
However, numerous areas of research are currently applying bioprinting techniques to the printing of various types of human tissue, an important first step towards printing functional whole organs.
Skin tissue
Several studies to date have fabricated human skin via bioprinting. In each case, the bio-ink comprised donor keratinocytes (the primary type of cell found in the outermost layer of skin) and fibroblasts (cells that provide the structural framework for tissue) with scaffolding biomaterials.
These resulted in bioprinted skin tissue that was morphologically and biologically representative of in vivo human skin tissue. More recently, bioprinting techniques including melanin-producing cells have produced fabricated skin tissue with similar pigmentation as the skin cell donors.
Skin tissue bioprinting technology is not yet advanced enough to produce fabrications capable of replicating the complete physiology and anatomy of human skin. They cannot be vascularized or stimulate regeneration of nerves, hair follicles and sweat glands. However, skin bioprinting technology has huge potential to improve outcomes for wound healing and wound reconstruction.
Cardiac tissue
Cardiovascular disease (CVD) is a leading cause of mortality, accounting for one-third of all deaths and causing a significant burden of disease globally. One of the main causes of death for patients with CVD is myocardial infarction, and whilst heart transplantation is one therapeutic option, it is vastly limited by the lack of donor hearts.
Advances in bioprinting have demonstrated its viability for regenerating or replacing damaged cardiac tissue by creating fabricated constructs such as cardiac patches. For use in cases of severe myocardial infarction, cardiac patches can be used to improve the contractile force of the myocardium. Other bioengineered cardiac tissue has included creating pulsating tubular biological pumps, with the potential to support ventricular functions.
Ultimately, the goal for cardiac tissue bioprinting is the production of a compatible complete heart with the functional properties of a natural organ, and recent advances in stem cell and bioprinting technologies have brought this into the realm of possibility.
Many pieces of research have described protocols to produce a complete bioengineered heart, resulting in the production of the first bioprinted heart complete with blood cells, ventricles and vessels in 2019.
Corneal tissue
Blindness due to disease of the cornea is the fourth leading cause of blindness worldwide. As corneas have low thickness and do not require vascularization, they are an excellent candidate for bioprinting.
Recently a team of researcher were able to fabricate 30 viable corneas from one tissue donor, using a bio-ink containing collagen and stromal cells. The resultant printed cells showed viability after production and at day seven post-printing.
References and Further Reading
Datta, P., Barui, A., Wu, Y., Ozbolat, V., Moncal, K. K., & Ozbolat, I. T. (2018). Essential steps in bioprinting: From pre- to post-bioprinting. Biotechnology advances, 36(5), 1481–1504. https://doi.org/10.1016/j.biotechadv.2018.06.003
Gungor-Ozkerim, P. S., , Inci, I., , Zhang, Y. S., , Khademhosseini, A., , & Dokmeci, M. R., (2018). Bioinks for 3D bioprinting: an overview. Biomaterials science, 6(5), 915–946. https://doi.org/10.1039/c7bm00765e
Lewis, A., Koukoura, A., Tsianos, G. I., Gargavanis, A. A., Nielsen, A. A., & Vassiliadis, E. (2020). Organ donation in the US and Europe: The supply vs demand imbalance. Transplantation reviews (Orlando, Fla.), 100585. Advance online publication. https://doi.org/10.1016/j.trre.2020.100585
Varkey, M., Visscher, D. O., van Zuijlen, P., Atala, A., & Yoo, J. J. (2019). Skin bioprinting: the future of burn wound reconstruction?. Burns & trauma, 7, 4. https://doi.org/10.1186/s41038-019-0142-7
Wang X. (2019). Advanced Polymers for Three-Dimensional (3D) Organ Bioprinting. Micromachines, 10(12), 814. https://doi.org/10.3390/mi10120814
Further Reading
Last Updated: Dec 23, 2020