Carotid artery stenosis or coronary artery disease refers to a narrowing of the carotid arteries, which are the major arteries in the neck that supply the brain with blood from the heart. A common cause of the condition is atherosclerosis, which causes fatty deposits to build up in the inner walls of the blood vessels and ultimately narrow the lumen or space in the arteries.
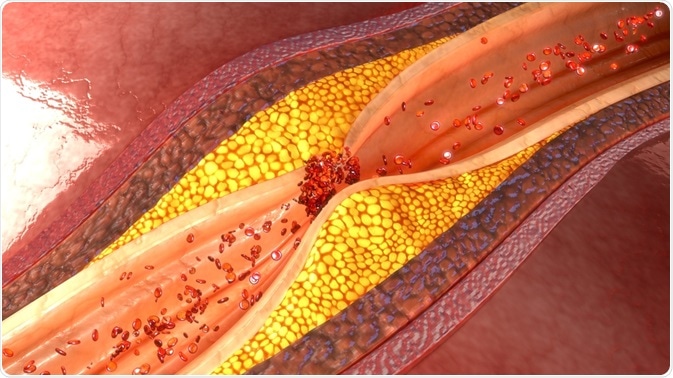
Image Credit: sciencepics / Shutterstock.com
Risk factors
Eventually, the carotid arteries can become completely blocked, which decreases blood flow to the brain and increases the risk of stroke. Carotid artery stenosis accounts for around 30% of stroke cases.
The likelihood of coronary artery stenosis developing is increased by certain risk factors including:
- High blood pressure
- Older age
- Diabetes
- Smoking
- Obesity
- Family history of atherosclerosis
- High cholesterol
- Lack of physical activity
Men who are younger than 75 years are at an increased risk of developing carotid artery stenosis as compared with women within this age range. After the age of 75, women are at a greater risk of the condition.
Symptoms
Patients with coronary artery stenosis do not usually present with any symptoms. Atherosclerosis progresses over time and fatty deposits build up in the arteries without causing any warning signs until the patient is at risk of transient ischemic attack (TIA), which is often the first sign patients present with.
A TIA is caused by a clot that has formed in the affected artery that dislodges and travels towards the brain, where it blocks a smaller artery. This can cause similar symptoms to those seen in stroke such as paralysis in one side of the body, difficulty speaking or responding, confusion, difficulty balancing, headache, and blurred vision.
Unlike a stroke, a TIA only lasts for a brief period and usually resolves within a few hours. However, the event is a warning sign that the patient is at risk of stroke, which can lead to severe disability and even death. Research has shown that people who have previously had a TIA are at ten times the risk of major stroke as compared with those who have not experienced a TIA.
Stroke Prevention - Carotid Artery Disease
Diagnosis
A diagnosis of carotid artery stenosis usually can include an initial assessment by a treating clinician, carotid ultrasonography, carotid angiography, a computed tomography (CT) scan, as well as a magnetic resonance angiography.
Initial health assessment
A healthcare provider will obtain the details of a patient's symptoms, their medical history, and also perform a physical examination. The doctor will be interested in any risk factors for carotid artery disease, as well as symptoms that indicate TIA.
The doctor may listen to arteries in the neck using a stethoscope to check for an abnormal sound referred to as a “bruit.” This sound can occur when blood flow is turbulent due to carotid artery disease. Detection of a carotid bruit usually leads to a referral for a carotid ultrasound to assess blood pressure and blood flow in the arteries.
In addition to this ultrasound, the healthcare provider may request CT or magnetic resonance imaging (MRI) scans to check for evidence of stroke or other damage. A CT angiography can also be prescribed, which is also used to assess blood flow in the arteries.
Carotid ultrasonography
Carotid ultrasonography is the most commonly used test for determining whether coronary artery stenosis is present. This is a non-invasive, painless technique that uses high-intensity sound waves to generate structural images of the carotid arteries.
This imaging technique is used to check for plaque build-up, blood clots, and narrowing of the arteries. The amount and velocity of blood that is moving through the vessels can be assessed using Doppler ultrasound.
Carotid angiography
Carotid angiography is an invasive procedure that involves the insertion of a catheter into a vein in the patient’s arm or leg that is subsequently guided towards the carotid arteries. A contrast dye is then passed through the catheter and real-time X-ray images of the arteries are taken. This enables a doctor to visualize the anatomy of these arteries and detect any abnormalities.
CT scan
A CT scan uses X-rays in conjunction with computer technology to generate detailed images of the head and neck. The technique can be used to generate cross-sectional two-dimensional (2D) and three-dimensional (3D) images of the carotid arteries and the brain.
The CT scan uses radiation to create images. Therefore, the risk to patients is weighed against the benefits before this procedure is performed.
Magnetic resonance angiography
Magnetic resonance angiography employs radio waves and magnetic fields to create detailed images of the carotid arteries and brain. This procedure can often detect even small cardiovascular events that have occurred in the brain. A contrast dye may also be used to highlight the arteries.
Next steps
If a patient is diagnosed with carotid artery disease, treatment is then initiated. The treatment will depend on how severe the stenosis is.
For some patients, lifestyle changes and medication may be sufficient to improve the condition. Comparably, other patients may require a minimally invasive procedure called carotid angioplasty and stenting to open up the artery. Some patients may require a more invasive intervention called carotid endarterectomy to remove the blockage in the artery.
References
- https://sherifsultan.ie/
- https://www.fmshk.org/
- https://www.mayfieldclinic.com/
- http://www.webmd.com/heart-disease/carotid-artery-disease-causes-symptoms-tests-and-treatment
- http://www.patient.co.uk/doctor/carotid-artery-stenosis
- https://www.nhlbi.nih.gov/
- http://www.radiologyinfo.org/en/info.cfm?pg=carotidstenosis
- http://www.mayoclinic.org/diseases-conditions/carotid-artery-disease/basics/tests-diagnosis/con-20030206
- https://www.secondscount.org/
Further Reading
Last Updated: Jul 13, 2023