Cirrhosis is a severe form of liver disease wherein normal liver tissue is replaced by scar tissue (fibrous tissue).
What changes occur in cirrhosis?
Cirrhosis or fibrosis of the liver can occur due to several liver-related diseases and conditions, such as hepatitis, non-alcoholic fatty liver disease, and excessive alcohol consumption. The replacement of healthy liver tissue with fibrous tissue leads to permanent liver damage, which is characterized by distorted blood flow through the liver and abnormal liver function.
Cirrhosis is a chronic liver condition that is often asymptomatic initially. The signs and symptoms start appearing when the liver is badly damaged. In some severe cases, cirrhosis can even lead to complete liver failure. In 2001, cirrhosis was estimated to be the fourteenth leading cause of death worldwide. With its increasing prevalence, it is likely to move up to the twelfth position by 2020. Adult men over 50 years are more susceptible to cirrhosis.
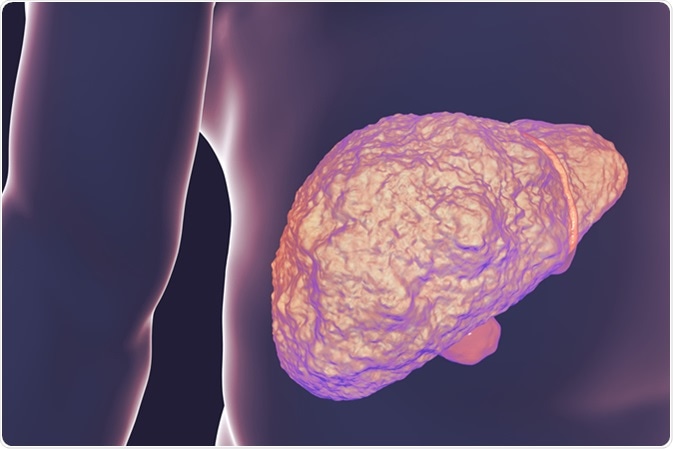
Liver with cirrhosis inside human body. 3D illustration. Image Credit: Kateryna Kon / Shutterstock
What causes cirrhosis?
Chronic liver damage due to a variety of diseases and conditions can ultimately lead to cirrhosis. The pathogenesis of cirrhosis can be triggered most commonly by viral hepatitis (hepatitis B, C, and D), non-alcoholic fatty liver disease, and alcoholic liver disease. Less common causes include genetic conditions such as hemochromatosis, cystic fibrosis, Wilson’s disease, biliary atresia, and glycogen storage disease. In addition, deficiency of a specific liver enzyme, Alpha-1 antitrypsin, can also cause cirrhosis.
Autoimmune diseases of the liver or bile duct, such as autoimmune hepatitis, primary biliary cholangitis, and primary sclerosing cholangitis, are other potential contributors to cirrhosis. In addition, Alagille syndrome, which is a genetic disease of abnormal bile duct functioning, can trigger the onset of cirrhosis.
The chronic consumption of certain medicines, such as pain killers, antipyretic drugs, and nonsteroidal anti-inflammatory drugs, may increase the chance of developing cirrhosis. In addition, frequent episodes of heart failure with liver congestion leading to disruption of the hepatic blood flow can lead to cirrhosis.
What are the signs and symptoms of cirrhosis?
In the initial stages, cirrhosis is mostly asymptomatic; however, the signs and symptoms start to appear as the disease worsens. The most common early symptoms of cirrhosis are weakness, loss of appetite, weight loss, nausea and vomiting, and abdominal pain.
At advanced stages, with severe liver injury, patients may experience confusion, lack of concentration, memory loss, mood changes, or sleep deprivation. Bruising and easy bleeding are also common at this stage.
People suffering from advanced cirrhosis may also experience swelling in the lower legs, ankles, or feet and abdominal bloating due to excessive fluid buildup. In some cases, yellowish tints appear in the skin and eyes (jaundice) and the urine becomes dark in color.
In women, loss of menstruation is frequently observed; in males, there may be loss of sexual drive, testicular atrophy, and gynecomastia (enlarged breasts).
Cirrhosis - Patient Stories
What are the common complications of cirrhosis?
Cirrhosis leads to disruption of the hepatic blood flow, leading to increased blood pressure in the portal vein (portal hypertension). This can subsequently trigger the accumulation of fluid in the legs and abdomen. Portal hypertension can also cause spleen enlargement and trapping of the leukocytes and platelets.
Due to portal hypertension, blood that should have drained through the portal system is often redirected to other smaller veins, which eventually leads to their rupture and bleeding. The rupture of the veins in the esophagus or stomach can lead to life-threatening bleeding.
People with cirrhosis are more likely to develop infections because of the reduced ability of the body to fight foreign invaders. As a consequence, these patients are more prone to urinary tract infections and pneumonia.
Since toxic substances are mainly metabolized in the liver, cirrhosis-related damage to the liver often leads to abnormal accumulation of toxins in the brain (hepatic encephalopathy), which subsequently causes confusion, difficulty thinking, and even unconsciousness.
Cirrhosis significantly increases the risk of liver cancer. In a large fraction of people, cirrhosis is the underlying cause of liver cancer. In some severe cases, cirrhosis may also lead to liver failure, in which the liver completely stops functioning.
How is cirrhosis prevented?
Although cirrhosis causes irreversible liver damage, timely diagnosis and treatment of the underlying condition may prevent the disease from getting worse. Thus the progression of the condition can be sometimes prevented by adopting certain preventive measures. Eating a healthy and balanced diet and avoid drinking excessive alcohol are among these useful steps.
Excessive accumulation of fat can induce liver damage. Thus, maintaining a healthy body mass index (BMI) is another important step in preventing cirrhosis.
Since the hepatitis virus is mainly transmitted via blood and semen, steps should be taken to avoid sharing needles or having unprotected sex.
From Cirrhosis to a Hepatitis C Cure | William's Story
Further Reading
Last Updated: Mar 19, 2019