Langerhans cell histiocytosis (LCH) is a rare condition characterized by abnormal growth of the Langerhans cells. The proliferation of these cells leads to the formation of tumors called granulomas, which can then invade the bones and cause pain, inflammation and (in some instances) bone fracture. The disease is most commonly seen in children younger than 15 years of age; however, it has been observed in other age groups too.
Skip to
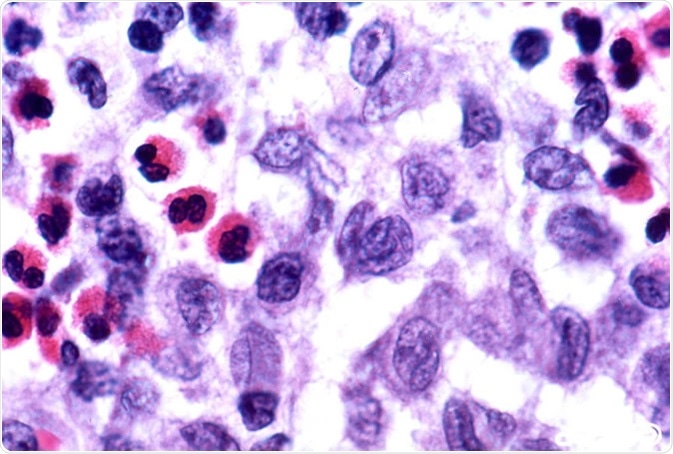
"Langerhans cell histiocytosis" by Pulmonary Pathology is licensed under CC BY-SA 2.0
Langerhans cell histiocytosis has a variable clinical presentation and usually initiates as a skin rash. It can also involve organs such as lungs, bone marrow, lymph nodes, spleen and the gastrointestinal tract.
The prognosis of the condition depends on the extent of the disease. If LCH is detected in the initial stage, prompt treatment can help to manage the disease well. Treating disease which has progressed represents a challenge, since any type of damage to the organs usually becomes a permanent complication.
Living with Langerhans Cell Histiocytosis
What are the causes of Langerhans cell histiocytosis?
The exact etiology of LCH is unknown; however, somatic mutations in the BRAF gene have been identified in the majority of the patients. In a nutshell, BRAF gene encodes a protein called B-Raf, which is involved in transmitting growth signals to the nucleus of the cell. Consequently, somatic mutations in the BRAF gene lead to increased production of the B-Raf protein, which ultimately causes uncontrollable cell proliferation.
Studies have also demonstrated the involvement of certain environmental toxins and virus in the development of LCH. Considering the latter, the most commonly implicated viruses are herpesviruses, but the studies on this topic are not yet conclusive.
What are the signs and symptoms of Langerhans cell histiocytosis?
LCH can exist either as an isolated skin or bone disease, or it can progress to a condition which involves multiple organs (most notably lung, liver, bone marrow and endocrine system).
The rash is the most common symptom associated with LCH. LCH rash has certain peculiar characteristics which aid in differentiating it from other skin disorders such as atopic dermatitis. The rash has scaly papules and hard nodules, while petechiae and crusted bloody scales are some other specific features which can help in differential diagnosis.
Bone involvement (which leads to pain and swelling of the affected body part) has been reported in the majority of the LCH patients. Bone lesions are most commonly observed in the hips, skull or ribs.
Pituitary gland is also affected in some cases. The damage leads to abnormalities in the hormones produced by the gland, which may result in problems such as diabetes insipidus, thyroid dysfunction, delayed puberty and/or infertility.
Pulmonary involvement can lead to blocked airways and breathing problems. This can also increase the risk of infections. Furthermore, bone marrow involvement can cause pancytopenia or reduction in the number of blood cells, which may lead to fatigue, increased infections and blood clotting problems. Lymphadenopathy and hepatosplenomegaly are some additional complications associated with LCH.
How is Langerhans cell histiocytosis diagnosed?
Physical examination and medical history to assess general health is usually the first step in establishing adequate diagnosis. Laboratory tests to check the complete blood count (CBC), blood chemistry, liver function test and urine analysis are also pursued. Moreover, BRAF gene testing is recommended to check for mutations in the BRAF gene. Water deprivation test may be done to diagnose cases of diabetes insipidus caused by LCH.
Bone scan and skeletal survey (with X-rays) may be done to check the bones in the body. Computed tomography (CT) scan, MRI (magnetic resonance imaging) and PET scan (positron emission tomography scan) are some additional imaging techniques which may aid in diagnosis. Finally, the assessment of the skin biopsy can help to confirm the diagnosis.
How is Langerhans cell histiocytosis treated?
Treatment strategy for LCH is decided after considering the extent of disease, the body parts that are affected and the amount of risk involved. Single-system LCH involves only a single body part, whereas multisystem LCH involves two or more organs.
The treatment usually entails the use of chemotherapy to stop the proliferation of abnormal cells. Curettage may be used to scrape of LCH cells from the bone. In cases where there is a severe organ damage, organ replacement may be a viable option.
Radiation therapy can be used to treat the skin lesions in LCH. Phototherapy such as combined psoralen and ultraviolet A (PUVA) therapy is also an effective treatment option to kill cancer cells in the skin tissues.
Immunotherapy is a novel treatment which uses an individual’s immune system to fight cancer. Steroids can be used to treat LCH lesions, while bisphosphonate therapy is recommended for bone problems. Anti-inflammatory drugs are used to treat the symptoms of pain and swelling. Finally, retinoids may help to halt the growth of LCH cells in the skin.
Further Reading
Last Updated: May 17, 2019