Introduction
Types of Ocular Melanoma
Cause and Risk factors
Symptoms
Genetics
Epidemiology
Diagnosis and treatment
References
Further reading
Ocular melanoma is the most prevalent type of cancer affecting the eye. It is known as the second most common type of melanoma. It occurs in pigment-producing cells. Melanocytes in the conjunctival membrane and uveal tract of the eye produce it. Uveal melanoma, or eye melanoma, is another name for ocular melanoma.
Although the vast majority of ocular melanomas are primary, metastatic melanoma from a primary cutaneous location can occur. Uveal and conjunctival melanoma are two types of ocular melanoma. Clinical examination is used to make a diagnosis in the majority of cases.
Image Credit: Lightspring/Shutterstock
Types of Ocular Melanoma
Uveal and nonuveal ocular melanoma are two types of ocular melanoma. The most common type of ocular melanoma is uveal melanoma, which includes choroid, ciliary body, and iris melanoma. When compared to iris or anterior uveal melanoma, choroidal and ciliary body melanoma are collectively referred to as posterior uveal melanoma. The most uncommon uveal melanoma is iris melanoma.
All conjunctival melanomas are nonuveal melanomas (CM). Melanocytes in the basal layer of the conjunctival membrane's epithelium give rise to conjunctival melanomas. Conjunctival melanoma is extremely rare, accounting for around 5% of all ocular melanomas.
Cause and Risk factors
In most cases, the cause of ocular melanoma is unknown. However, there are several risks to be aware of. Predisposing factors for uveal melanoma include congenital ocular and oculodermal melanocytosis, as well as a uveal nevus. Other host susceptibility factors like light eye color, fair skin color, and difficulty to tan have been linked to an elevated risk of uveal melanoma, according to a meta-analysis. Atypical cutaneous nevi, cutaneous freckles, common cutaneous nevi, and iris nevi have also been linked to an increased risk of uveal melanoma development. Occupational cooking has also been indicated as a factor that increases the incidence of uveal melanoma.
Conjunctival melanomas can develop spontaneously or as a result of a pre-existing condition such as primary acquired melanosis (PAM) or conjunctival nevus. PAM is responsible for about 60% of conjunctival melanomas. Other common risk factors for ocular melanoma include old age and being of Caucasian descent.
Symptoms
The appearance of uveal melanoma is mostly determined by the tumor's size and location. It can range from asymptomatic, discovered by chance during an eye checkup, to various visual abnormalities and eventually total loss of sight in the affected eye. Blurred vision, photopsia, visual field defect, discomfort, and pain are the most prevalent symptoms. Metamorphopsia, floaters, and redness, are also possible. Ciliary body melanoma is a dome-shaped or sessile lesion that can be seen with a dilated pupil. Iris melanoma is usually asymptomatic and presents as the development of an iris lesion.
Melanoma of the conjunctiva usually appears as an elevated pigmented lesion surrounded by conspicuous feeder blood vessels or patches of PAM. Patients report pigmented spots or lumps as the most prevalent symptom, although irritation and pain are uncommon.
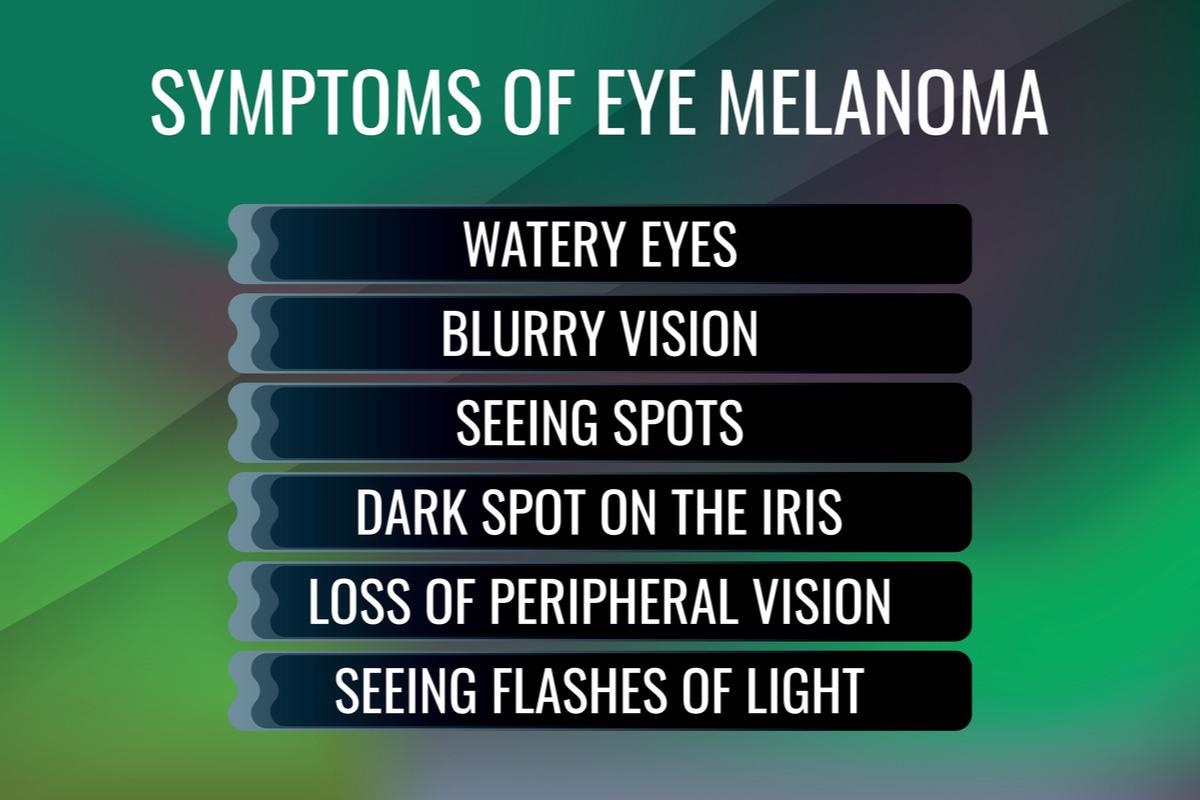
Image Credit: A-H-K/Shutterstock
Genetics
Cancer cells' genetic instability is characterized by chromosomal abnormalities. GNA11 and GNAQ are the most frequently mutated genes in UM. These genes are mutated in 71–93 % of all UM cancers. In the great majority of cancers, GNAQ and GNA11 are mutually exclusive in the G signaling pathway. BAP1, SF3B1, and EIF1AX are also frequently altered genes in UM. BRAF mutations are seen in 25% to 35 % of conjunctival melanoma cases, with the BRAF V600E variant accounting for the vast majority. The BRAF gene is important in signal transduction and has been found to be mutated in a variety of cancers, the most frequent of which is malignant melanoma.
Epidemiology
Ocular melanoma is the second most prevalent type of melanoma, yet it is still uncommon, accounting for only 3.7 percent of all melanoma occurrences. White individuals have an 8-10 times higher rate of ocular melanoma than black individuals. Ocular melanoma has a prevalence of 6 per million in the United States, compared to 153.5 per million for cutaneous melanoma. It is more frequent in men, with a 6.8 per million incidence rate compared to 5.3 per million in women. The ratio of males to females is 1.29. Ocular melanoma is more common in Australia, with an incidence of 8 per million in men and 6.1 per million in women.
In the United States, the rates of uveal and conjunctival melanomas are 4.9 and 0.4 per million, respectively. In Europe, uveal melanoma incidence decreases from over 8 per million in northern countries to less than 2 per million in southern countries, indicating a north-to-south gradient. Uveal melanomas occur at a rate of about 7 per million Caucasians per year. Presentation peaks at about sixty years of age and is uncommon before adulthood. Conjunctival melanoma is becoming more common, especially among white males over the age of 60.

 Read Next: Malignant Melanoma
Read Next: Malignant Melanoma
Diagnosis and treatment
After a thorough clinical examination, eye examinations, including slit-lamp biomicroscopy, are used to diagnose uveal and conjunctival melanoma. Other approaches for diagnosing uveal melanoma include indirect ophthalmoscopy and ancillary diagnostic testing (ultrasonography, fluorescein angiography, and optical coherence tomography). The accuracy of clinical examination-based diagnosis is currently exceedingly high, at around 99 percent.
Surgery, radiation, or a combination of these therapies are used to treat primary UM. Enucleation, resection, radiation, and proton beam therapy are options for treating pediatric UM, just as they are for adults. Wide local excision plus adjuvant therapy, such as cryotherapy, brachytherapy, and topical chemotherapeutic drug administration, is the current standard treatment for conjunctival melanoma. Unfortunately, there is no known treatment for ocular melanoma metastatic illness. More genetic and molecular testing is required to acquire a better understanding of ocular melanoma and, perhaps, to identify treatment targets.
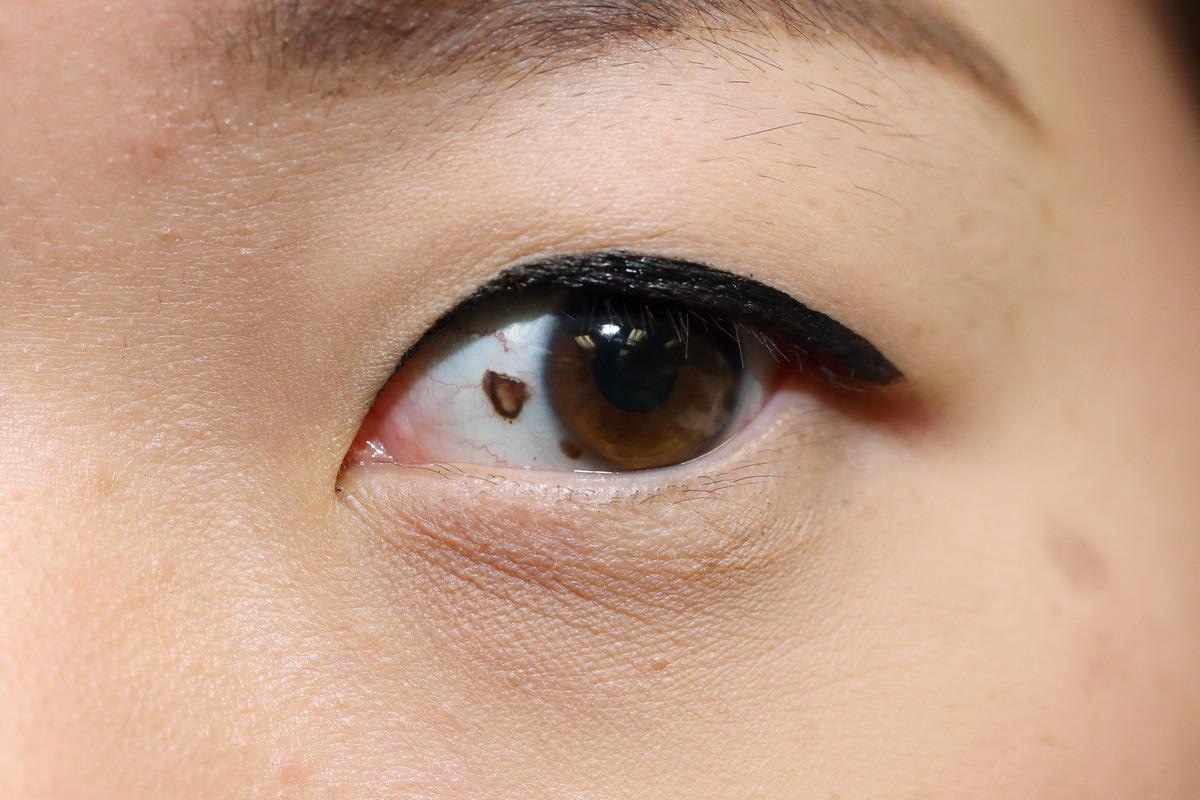
Suspicious mole presenting on the eye. Image Credit: charnsitr/Shutterstock
References
- van Poppelen, N. M., de Bruyn, D. P., Bicer, T., Verdijk, R., Naus, N., Mensink, H., Paridaens, D., de Klein, A., Brosens, E., & Kiliҫ, E. (2020). Genetics of Ocular Melanoma: Insights into Genetics, Inheritance and Testing. International journal of molecular sciences, 22(1), 336. https://doi.org/10.3390/ijms22010336
- Balasubramanya, R., Selvarajan, S. K., Cox, M., Joshi, G., Deshmukh, S., Mitchell, D. G., & O'Kane, P. (2016). Imaging of ocular melanoma metastasis. The British journal of radiology, 89(1065), 20160092. https://doi.org/10.1259/bjr.20160092
- Jovanovic, P., Mihajlovic, M., Djordjevic-Jocic, J., Vlajkovic, S., Cekic, S., & Stefanovic, V. (2013). Ocular melanoma: an overview of the current status. International journal of clinical and experimental pathology, 6(7), 1230–1244.
- What is Ocular Melanoma? [Online] American association of Ophthalmology. Available at: https://www.aao.org/eye-health/diseases/what-is-ocular-melanoma
- Ocular (eye) melanoma. [Online] Cancer council. Available at: https://www.cancer.org.au/cancer-information/types-of-cancer/rare-cancers/eye-ocular-melanoma
Further Reading
Last Updated: May 23, 2022