As with any biochemical system, viruses are sensitive to temperature extremes that denature their constituent proteins and disable the functional aspects of the organism.
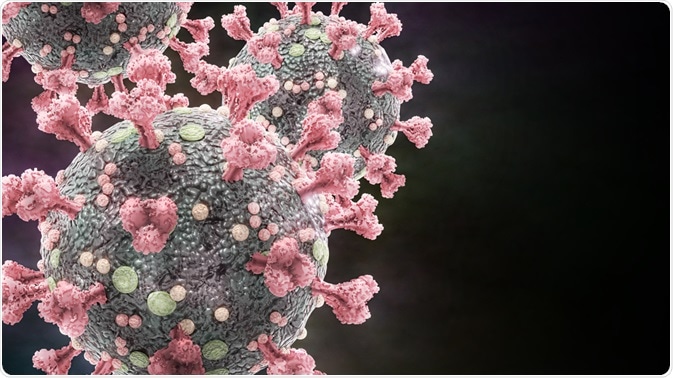 Image Credit: Dotted Yeti/Shutterstock.com
Image Credit: Dotted Yeti/Shutterstock.com
Several factors influence the temperature that may inactivate a virus, including specifics of the structure of the particular virus, the test matrix employed, its pH and ionic strength, and environmental humidity. The stability of the virus protein shell, state of virus aggregation, and access to surface receptors are each regulated by these factors, which subsequently alters the thermal inactivation temperature.
A virus may contain single or double-stranded DNA or RNA, and may or may not be coated with a lipid envelope around the protein capsid, which are also affected differently by temperature.
How does heat inactivate viruses?
Two primary mechanisms of inactivation have been identified across numerous viruses: enzymatic degradation of unprotected viral nucleic acids at temperatures of around 40⁰C, and destruction of externally facing proteins in complete viruses at higher temperatures.
Many viruses are effectively sealed by a protein shell known as a capsid, which when broken by degradation or conformational changes can allow the escape of the viral genome contained within. Controlled heat treatment experiments have demonstrated this, as an empty capsid shell is generated, and small pores in the hollow capsid shell are often visible following heat treatment, making the route of expulsion of the nucleic acids evident.
At the intermediate stage of heating, nucleic acids are still present within the capsid but are bound with nucleoproteins that maintain stability. Interestingly, these nucleic acids can remain stable at comfortable pH levels thanks to these proteins, with single-stranded RNA being less stable than dsRNA, ssDNA, or dsDNA, in that order.
Is SARS-CoV-2 sensitive to heat?
Some studies have suggested that coronaviruses in general are particularly sensitive to thermal damage, as the membrane and nucleocapsid proteins are easily affected by heat. A literature study recently assembled by Kampf, Voss, and Scheithauer (2020) collated ten studies of heat inactivation against SARS-CoV-2.
Overall, 60⁰C for 30 minutes, 65⁰C for 15 minutes, or 80⁰C for 1 minute was found sufficient for thermal disinfection, defined as a 99.99% (4 log10) loss in infectivity. The primary mechanism, as with most other viruses, was denaturing of the nucleocapsid proteins. In most cases, the capsid was completely denatured at 55⁰C after 10 minutes, though further heating ensures that a greater proportion of the virus particles are affected. The authors note that each of these tests was performed in solution, and thus dry heating may induce denaturing at a different rate.
Mathematical models developed by Seifer & Elbaum (2020) aimed to assess the inactivation of SARS-CoV-2 at physiologically relevant temperatures, i.e. around 40⁰C, and at mild extremes of up to 60⁰C. In cell culture SARS-CoV-2 showed a 99.99% fold reduction in activity after incubation at 56⁰C for 15 minutes, which was in line with the predictions made by the mathematical model, lending some credence to the work. At a normal body temperature of 37⁰C, the model predicts 99.99% inactivation after 48 hours, while a mildly elevated temperature of 39⁰C is expected to induce 99% inactivation at 14 hours, increasing to 99.99% inactivation after 28 hours.
At higher temperatures, the group noted that the wettability of the capsid proteins played an influential role in the rate of degradation observed, with less hydrophobic proteins coming into better surface contact with water molecules. Therefore, the medium in which the virus is located can directly alter the degradation temperature, as pH and ionic strength influence wettability. With wetting, the system entropy is reduced as a greater degree of thermal energy is available to the system through molecule-molecule contact, meaning that lower temperatures impart a similar effect.
Interestingly, SARS-CoV-1 particles exposed to the same conditions as SARS-CoV-2 appear to be less easily inactivated, though the reason for this is not yet completely clear. Some associations have suggested that the sauna could be useful as a COVID-19 preventative, as the air temperature can often reach over 85⁰C, with temperatures in the trachea reaching 45⁰C.
However, according to the mathematical model discussed above, one would need to remain in the sauna for over 7 hours, which could be damaging to health in many other ways. 15 minutes at this temperature, they suggest, could inactivate as much as 30% of the virus in the accessible respiratory tract, though there are no studies supporting this at this time.
Heat is a cheap and widely accessible disinfectant that has several advantages over many chemical-based disinfectants. Pathogens cannot develop significant resistance to extreme heat, though such therapies are difficult to apply to any living system. Uncovering the precise mechanism behind thermal inactivation of SARS-CoV-2 will enable more efficient disinfection of objects that can undergo heat treatment, and optimizing this procedure may relieve some of the burden placed on healthcare providers around the world with regards to PPE regeneration and supply during the course of the pandemic.
Sources
- Knight, A. I., Haines, J. & Zuber, S. (2013) Thermal inactivation of animal virus pathogens. Virology, 11. www.researchtrends.net/.../article_pdf.asp
- Kampf, G., Voss, A., & Scheithauer, S. (2020) Inactivation of coronaviruses by heat. Journal of Hospital Infection, 105(2). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7271332/
- Seifer, S. & Elbaum, M. (2021) Thermal inactivation scaling applied for SARS-CoV-2. Biophysical Journal, 120. https://www.cell.com/biophysj/pdf/S0006-3495(20)33166-0.pd
Further Reading
Last Updated: Mar 22, 2021