Overview
Cytopathology is the use of specialist diagnostic techniques to examine individual cells extracted from tissues to determine the cause and nature of a disease.
Cell samples may be gathered during routine diagnostic tests, such as bronchoscopy and cystoscopy. Specific tests, such as the Papanicolaou test, also known as the Pap test or fine-needle aspiration, can be used to gather cells from specific sites for diagnosis.
Analysis of cell samples is often a rapid process, but requires specialist training to correctly identify cells that pose potential danger to a patient, such as pre-cancerous, cancerous or infected cells. This is the job of a trained cytopathologist; a medical doctor who has undergone additional training to correctly review and interpret the results from cytopathology tests.
The first test developed in the field of cytopathology was the Pap test. It is widely considered to be the most successful screening test in medical history, and remains a vital part of modern cytopathology.
Cytopathology has since played a key role in clinical diagnosis of cancerous and pre-cancerous disease states, benign tumors, and some infectious diseases. The field now encompasses a wide range of techniques for a variety of tissues.
The Pap test
The Pap test is a diagnostic technique that utilizes a sample of cells taken from the cervix. Two methods can be used in a Pap test; conventional and automated liquid tests.
In a conventional Pap test, cells are placed on a glass slide, and then fixed and stained with a combination of dyes. The cells are inspected using light microscopy for abnormalities, such as morphological or nuclear feature changes.
In the newer automated liquid Pap test, cell samples are placed in a vial of preservative for analysis. This screening method has proven to be more efficacious in diagnosis when compared to a traditional Pap test.
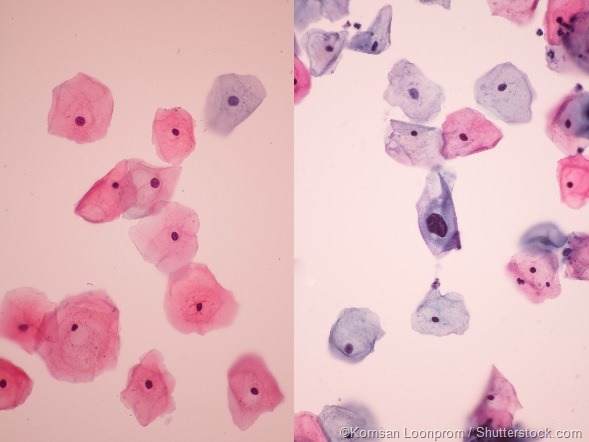
The images above show two examples of results from a standard Pap test. Cells that are cancerous or pre-cancerous are clearly distinct from normal samples.
Pap tests are the most cost-effective method for the detection and prevention of cervical cancer. Since the introduction of the method in the 1930s, cervical cancer mortality rates have fallen by 70%.
Its success can be attributed to the simplicity of the technique, the low cost, and low false-negative rate. Current guidelines in the US recommend that women receive their first Pap test at age 21, and are screened regularly every 3–5 years after that.
The Pap test is being phased out in favor of the Human Papilloma Virus (HPV) DNA or RNA screen. This test has been shown to have a higher success rate identifying cells infected with HPV, which is a risk factor for cervical cancer.
Fine-needle aspiration biopsies
The other principal diagnostic tool of the cytopathologist is the fine-needle aspiration biopsy. This technique uses a thin needle to remove a sample of cells from just beneath a patient’s skin.
As with the Pap test, these cells can be fixed, stained and examined under a microscope.
How a fine needle aspiration breast biopsy is taken | Bupa Health
Fine-needle aspiration allows for the sampling of a wide range of tissues at minimal discomfort to the patient, and is often the best diagnostic strategy when investigating a potentially cancerous or pre-cancerous lesion.
However, fine-needle aspiration has been criticized for the unnecessarily high risk associated with its use. In a report in the British Medical Journal in 2004, it was estimated that 0.4–5.1% of procedures undertaken to investigate liver lesions caused needle tract metastases, which is the spreading of cancer cells along the path of the needle. Needle tract metastases have also been recorded in pulmonary, prostate, and breast cancer cases.
Despite this, the procedure remains an invaluable diagnostic aid, and is frequently the first choice of medical professionals when investigating a possible cancer diagnosis.
References
-
American Society of Cytopathology. About cytopathology. https://cytopathology.org/. Accessed 11 June 2016.
- National Cancer Institute. Pap and HPV testing. http://www.cancer.gov/types/cervical/pap-hpv-testing-fact-sheet. Accessed 11 June 2016
- National Cancer Institute. Cervical Cancer Screening (PDQ®)–Health Professional Version. http://www.cancer.gov/types/cervical/hp/cervical-screening-pdq. Accessed 11 June 2016
- Cramer DW. The role of cervical cytology in the declining morbidity and mortality of cervical cancer. Cancer 1974; 34: 2018–2027
- Karimi-Zarchi M, Peighmbari F, Karimi N et al. A Comparison of 3 Ways of Conventional Pap Smear, Liquid-Based Cytology and Colposcopy vs Cervical Biopsy for Early Diagnosis of Premalignant Lesions or Cervical Cancer in Women with Abnormal Conventional Pap Test. Int J Biomed Sci 2013; 9 (4): 205–210
- Michael CW. The Papanicolaou Smear and the Obstetric Patient: A Simple Test with Great Benefits. Diagn Cytopathol 1999; 21 (1): 1–3
- Sankaranarayanan R, Nene BM, Shastri SS et al. HPV Screening for Cervical Cancer in Rural India. N Eng J Med 2009; 360 (14): 1385–1394
- Pitman MB and Layfield LJ. Guidelines for Pancreaticobiliary Cytology from the Papanicolaou Society of Cytopathology: A Review. Cancer Cytopathol 2014; 122 (6): 399–411
- Metcalfe MS, Bridgewater FGH, Mullin EJ and Maddern GJ. Useless and dangerous — fine needle aspiration of hepatic colorectal metastases. BMJ 2004; 328 (7438): 507–508
- Chen GL, Chian CF. Needle tract pulmonary metastases. QJM 2015; 108 (10): 837–838
- Volanis D, Neal DE, Warren AY, Gnanapragasam VJ. Incidence of needle-tract seeding following prostate biopsy for suspected cancer: a review of the literature. BJU Int 2015; 115: 698–704
- Bott S, Mohsen V, Wells C, Carpenter R. Needle tract metastases in breast cancer. Eur J Surg Oncol. 1999; 25 (5): 553
Last Updated: Jul 19, 2023