Jul 26 2013
Adaptimmune announced today that it has opened a Phase I/IIa, multiple-site, two-cohort, open-label clinical trial in ovarian cancer at Roswell Park Cancer Institute (RPCI) in Buffalo, N.Y., and City of Hope (COH) in Duarte, Calif.
Researchers will investigate the safety, bioactivity and effectiveness of treating patients with their own T cells after genetically engineering the cells to enhance their anti-tumor properties.
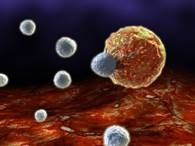
T cell killing a tumor cell
“T cells are the foot soldiers of the human immune system, attacking invaders like bacteria, viruses and cancer,” says Kunle Odunsi, MD, PhD, Director of RPCI’s Center for Immunotherapy and the study chair. “We believe that by modifying the T cells so that they express a high-affinity receptor for a protein that is a known cancer/testis (CT) antigen, we can fully exploit their ability as cancer killers.”
During the trial, T cell receptors (TCRs) that have been developed using Adaptimmune’s unique TCR enhancement technology will be deployed to target two CT antigens, NYESO-1 and LAGE-1. They will be transferred to the patients’ T cells in a process for autologous T cell manufacturing developed by Carl June, MD, and Bruce Levine, PhD, at the Perelman School of Medicine at the University of Pennsylvania, Pa., and then licensed to Adaptimmune. Manufacturing will be performed centrally by Progenitor Cell Therapy in Allendale, N.J.
Adaptimmune is the regulatory sponsor, owns the core T cell receptor technology, and is funding the study. Dr. Odunsi is the lead clinical investigator at RPCI and protocol Chair. Mihaela Cristea, MD, associate clinical professor, Medical Oncology, is the lead clinical investigator at City of Hope.
The study is opening on the heels of promising clinical data emerging in sarcoma and myeloma studies, where the same engineered T cell product is under investigation. Interim data from these studies was presented at the American Association for Cancer Research Annual Meeting in March and American Society for Cell and Gene Therapy Annual Meeting in May of this year.
Ovarian carcinoma is the fourth-most-common cancer in women, accounting for approximately 22,000 new cases and 15,000 deaths per year in the United States. With standard therapy, long-term response rates are low, and the five-year survival rate for advanced ovarian cancer is only 30%. The clinical trial focuses on this unmet medical need and will include patients who are resistant to chemotherapy and/or have received more than two lines of chemotherapy for their ovarian cancer.
Infusion of the CT antigen-specific T cells will occur following a brief treatment with relatively high dose of “lymphodepleting” chemotherapy to prepare the patient’s immune system for the gene-modified T cells. Previous clinical trials for different cancer indications have demonstrated that the lymphodepleting chemotherapy procedure is safe and promotes reconstitution of the immune system with the gene-modified T cells.
Dr. Odunsi is also the Chair of Gynecologic Oncology at RPCI and has been studying NY-ESO-1 vaccines in immunotherapy clinical trials for ovarian cancer patients since 2002. “NY-ESO is a very promising tumour antigen that I have worked with for years under the umbrella of the Cancer Vaccine Collaborative (CVC) Program of the Cancer Research Institute and the Ludwig Institute for Cancer Research,” says Dr. Odunsi. “This technology basically allows us to genetically engineer a powerful T cell response in patients against the NY-ESO-1 antigen, which is very exciting.”
Stephen J. Forman, MD, director of the T Cell Therapeutics Research Laboratory at City of Hope, initially brought the Adaptimmune technology to City of Hope due to his long-standing interest in adoptive and engineered T cell therapy for cancer. “The evaluation of this therapy in both hematologic and solid tumors will help us to understand the function of the engineered T cells in different tumor settings,” says Dr. Forman, chair of the Department of Hematology & Hematopoietic Cell Transplantation and holder of the Francis and Kathleen McNamara Distinguished Chair in Hematology and Hematopoietic Cell Transplantation. “I’m very enthusiastic to have this study join our programs at City of Hope, and to be able to offer our patients these novel and promising therapies.”
A myeloma study using this technology is also planned at the site.
A total of six patients will be enrolled in the ovarian trial. Only patients capable of responding to the therapy — those with the correct tissue marker (HLA-A*0201) and whose tumor expresses NY-ESO-1 and/or Lage-1 — will be enrolled. Enrollment is expected to complete within six to nine months. If data are promising, the study may be extended to include more patients.
“We are enormously pleased to be working with world leaders in immunotherapy for cancer,” says James Noble, CEO of Adaptimmune. “Ovarian cancer is an important clinical indication with which to evaluate our CT antigen specific TCRs because of the dismal prognosis of current standard care for advanced ovarian cancer, so the effects of the T cell immunotherapy can be rapidly assessed.”
Additional study details and contact information for patients interested in finding out more about participation can be found at clincialtrials.gov, under trial identifier number NCT01567891.
Both City of Hope and Roswell Park Cancer Institute are National Cancer Institute-designated Comprehensive Cancer Centers.
Source: http://www.adaptimmune.com/