Psoriasis is a long-term skin condition caused when certain immune cells – T cells – are triggered and become overactive. These T cells act as if they are healing a wound and cause the rapid growth of skin cells, resulting in the build-up of ‘plaques’ of psoriasis on the skin’s surface which can then flake, bleed and cause itching or burning sensations.
The disease burden of psoriasis on patients often goes far beyond physical symptoms, frequently impacting on emotional wellbeing and in some people is associated with depression, anxiety and suicidal thoughts, particularly in those affected with severe psoriasis. The emotional and physical elements of psoriasis are very much connected, and so both must be considered in any treatment plan.
Treating psoriasis can be a big challenge for HCPs. Patients with mild psoriasis can often be managed in primary care using creams and ointments, however patients with moderate to severe disease, or people in whom psoriasis is having a major effect on their lives, need to be referred to a dermatologist for specialist care. It is essential that all patients receive regular review in order to assess disease progression, comorbidities and responses to treatment.
If patients are referred to secondary care, there are a variety of effective treatments available for dermatologists to prescribe. It is important to remember that everyone’s experience with psoriasis is different, patients may respond differently to particular treatments whilst suitability of treatments vary from patient to patient.
As a dermatologist, it is my job to support my patients and understand what is important to them with regard to their psoriasis and their treatments and also how their psoriasis affects their lives physically, socially and psychologically. The choice of treatment is then targeted towards individual needs and preferences and we work together to achieve patient’s individual goals.
A major challenge around treating psoriasis is communication - psoriasis can flare and resolve in between appointments so it can be difficult to express and describe the life impact of these flares and recall possible triggers and response to treatments. People with psoriasis can also find it very difficult to talk about their emotions – something known as alexithymia – again making it difficult for clinicians to fully appreciate the impact of psoriasis.
Why do the symptoms of psoriasis often fluctuate?
Whilst we know psoriasis symptoms are caused by an immune response, it is not yet clear what initially triggers that response to take place. Research suggests that a flare up can be caused by injury to the skin, stress or anxiety, hormonal changes, drugs or certain infections.
How can these challenges be overcome?
The best way to overcome these challenges and optimise patient experience and outcomes is to ensure regular review and assessment alongside improving communication between patients and their doctors. Due to the individual nature of psoriasis, effective treatment is about going on a journey with a patient, regularly assessing the condition and reviewing treatment options accordingly.
Improving communication between doctor and patient is vital so that the doctor can be given all the relevant information, particularly how the condition has fluctuated or responded to treatments in between appointments, rather than just having a snapshot on a particular day. Understanding which triggers are relevant to individual patients helps prevent flares and achieve a more consistent improvement.
Communication is also important for a doctor to be able to assess the psychological impact that the psoriasis is having so they can provide appropriate advice and support.
One tool that can help patients and doctors is PsoriASSESS. This tool helps patients to track their condition and communicate their experience more effectively, and gives doctors better insights into their patients’ condition to improve clinical management.

Please can you give a brief overview of PsoriASSESS?
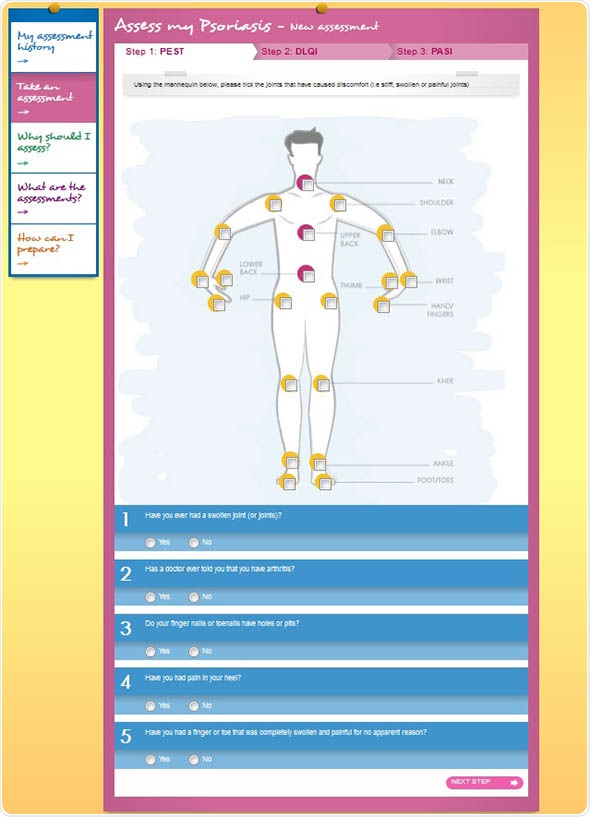
PsoriASSESS is a clinical, integrated psoriasis website for both patients and dermatologists. Its goal is to provide a more objective picture of the condition, both good and bad, over the time between consultations so that the dermatologist can better assess, diagnose and treat a patient’s psoriasis. Through the website, patients can take quick and easy self-completion questionnaires as well as compile a regular diary, complete with pictures of their psoriasis as it fluctuates over time.
With the patient’s permission, this data is available to the dermatologist through the NHS IT system. This means that dermatologists can evaluate and assess patients with more information than through the normal consultation approach where only a snapshot of the psoriasis is available. This will lead to more appropriate and informed treatment decisions.
How long do the recommended assessment tests take to complete?
Not long at all. The self-completion tests used on PsoriASSESS are all validated tools that are designed to be intuitive and user friendly for patients. The information they provide to dermatologists is really useful in assessing severity and informing treatment decisions.
What impact do you think tools like PsoriASSESS will have on clinical decision-making and do you think it will change the doctor-patient relationship?
It can sometimes be hard for a doctor to truly appreciate how psoriasis is affecting the lives of their patients between consultations, especially when the patient might find it hard to express or measure how the condition varies.
By linking a patient’s diary and online self-assessment results with the NHS IT system, psoriASSESS provides doctors with information that reflects the true nature of a person’s psoriasis as it fluctuates. This enables more open communication between an individual and their doctor which in turn informs clinical decisions and helps doctors to set more patient-centred treatment goals and timelines.
As dermatologists are familiar with the tools being used, it can also save time in an appointment, allowing the dermatologist to spend more time consulting with the patient to discuss the results of assessment tools, treatment options and patient-derived treatment goals. It may also ensure the regular use of assessment tools to assess response to treatment.
What are the main benefits and challenges associated with the move towards greater patient involvement in tracking and understanding their conditions between consultations?
Informed patients generally are much better at communicating about their condition and more likely to play an active role in managing their health - which is a great help for doctors.
Support services that help people track and create a personal record of these changes, like PsoriASSESS, help them to feel more in control which can lead to a greater sense of empowerment and confidence. This may in turn improve adherence to treatment and appropriate escalation or change in medication when necessary.
In what ways would you like to see PsoriASSESS improved going forwards?
PsoriASSESS has been developed in collaboration with dermatologists such as myself and so has been designed specifically to aid our contact with psoriasis patients. The nature of the tool is that the more patients use it then the more clinicians can build a fuller understanding of their patients’ condition.
I’d hope that in the future models like this can be applied to other long term conditions, allowing better information sharing between doctors and their patients, and aiding effective and sustainable management of long term conditions. I would also hope that the management of long-term conditions becomes more of a shared decision making process between patient and clinician.
And what can be done to help patients overcome the psychological impact of psoriasis?
The psychological impact of psoriasis is often unrelated to physical severity, and therefore it is important for doctors to discuss and assess emotional wellbeing with their patients irrespective of physical symptoms. Patients who are experiencing distress should relieve appropriate and timely support and psychological intervention if necessary.
I am a member of the See Psoriasis: Look Deeper (SPLD) collaboration which aims to raise awareness of the psychological and social impact of psoriasis. By raising awareness, we hope that this will encourage doctors and patients to address not only the physical effects of psoriasis, but also the associated co-morbidities, particularly the psychological and social impact of psoriasis.
SPLD has recently collaborated with NHS psychologists to create a series of psychological support booklets to help patients to manage some of the emotions and behaviours frequently associated with psoriasis. All of the booklets are free to download for patients or HCPs from the campaign website - www.seepsoriasislookdeeper.co.uk and are specifically tailored to the needs of people with psoraisis.
What do you think the future holds for psoriasis management?
Recent years have brought a much-needed array of effective treatments for psoriasis, which have transformed the lives of many people whose lives were previously ruined by psoriasis.
However, many patients with severe psoriasis are still not receiving timely effective treatment, resulting in unnecessary suffering and wasted lives. This is partly because there is still a lack of knowledge regarding the availability of effective treatments and lack of understanding of the, often devastating, life-impact of psoriasis. We also still have some way to go to address the multiple co-morbidities associated with psoriasis and the psychological and social impact of having this long-term skin condition.
I would hope that in the future all people with psoriasis receive timely appropriate effective treatment for their psoriasis, psychological support and intervention if needed and screening for associated conditions such as obesity, arthritis and diabetes.
Where can readers find more information?
The Psoriasis Association is the UK patient group for psoriasis, and has lots of information on its website, www.psoriasis-association.org.uk/
For more information about the psychological impact of psoriasis, and the See Psoriasis: Look Deeper website, our campaign website is www.seepsoriasislookdeeper.co.uk

About Dr Sandy McBride
Dr Sandy McBride is a Consultant Dermatologist with a special interest in psoriasis and the psychological impact of skin conditions. As well as performing general dermatology, she leads a multi-discplinary psoriasis service which aims to provide holistic care to people with psoriasis.
She is also Dermatology Lead for the Royal Free psycho-dermatology service, a member of the British Association of Dermatologists psycho-dermatology working party and the See Psoriasis: Look Deeper collaboration. Her research interests include the management of psoriasis and the psychological impact of psoriasis and other skin diseases.