Older people living in care homes fall three times more frequently than individuals who still live in their own homes. There is often debate over the idea of people going into care homes as a solution to the fact they are falling at home but they can still fall in the care home.
Furthermore, once a person falls, they're much more likely to have another fall because the fear of falling increases. When people become more scared of falling, they then become more likely to fall over.
What are the main causes of falls in care homes?
People living in care homes are much frailer than people living at home. They may also have more comorbidities such as stroke damage or dementia which may then be further complicated by a urinary tract infection, for example. These things often tend to occur as lots of different problems, as one thing on top of another.
Eighty percent of people living in care homes have a cognitive problem, so their memory, reasoning or spatial awareness may be impaired. They are then more likely to take risks that they wouldn’t otherwise take.
Also, when people have a cognitive problem, it can be very difficult to teach them how to use something. As people get older, we usually try and teach them how to use a walking stick or a walking frame, but it is much more difficult to teach people with dementia, which leaves them at a greater risk of falling over.
However, people fall for all sorts of reasons – because they trip on something, because there's something wrong with their blood pressure, because their legs are weak and can't support their body properly. Some people who have had a stroke have paralysis along one side of their body or they have a proprioceptive problem and can't feel their joints as well as they used to be able to.
Please can you give a brief introduction to GtACH (Guide to Action for falls prevention in Care Homes?
The GtACH was designed locally by researchers and clinicians who pulled together all the published literature on the measures people can take to help care home residents reduce their risk of falling over.
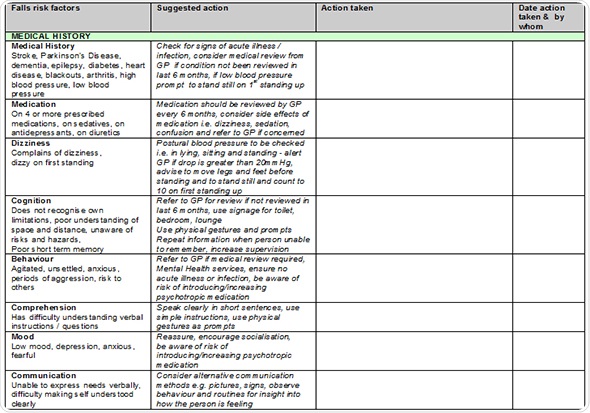
The GtACH is an assessment tool presented in a grid-like format with boxes that can be ticked to indicate the risk factors for falling. If someone is on more than four medications or has a problem with their eyesight or blood pressure, then the appropriate boxes will be ticked to indicate this.
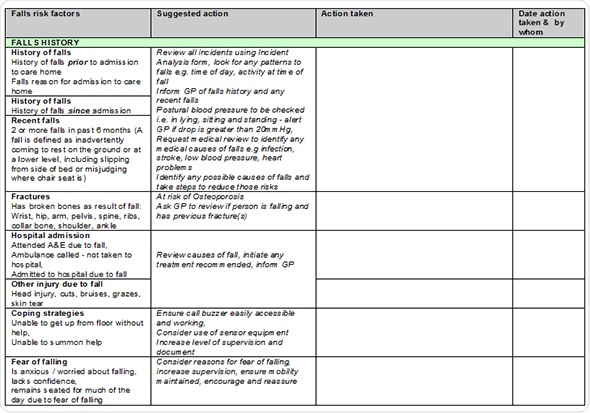 Also, the manual contains information about interventions to try and overcome these risk factors. It will tell you what to do if someone has a blood pressure problem, an eyesight problem or a problem drinking their fluids (inadequate fluid intake can also increase the risk of falling over).
Also, the manual contains information about interventions to try and overcome these risk factors. It will tell you what to do if someone has a blood pressure problem, an eyesight problem or a problem drinking their fluids (inadequate fluid intake can also increase the risk of falling over).
GtACH can therefore be used as a guide, as well as an assessment tool, which is why it's referred to as a guide to action. The guide is also written in a language that someone who has no medical training can understand.
We train the care home staff to use it and also provide them with a manual. If somebody is only having two drinks a day, for example, and they need to have at least six drinks a day to reducet their risk of falling over, we'll give the care home staff information containing ideas about how to get people to drink more fluids. Care home staff would then use that to devise a plan rather than being confused about what they need to do.
How is risk of falling assessed on an individual basis?
There are fall risk assessments available, but most of them have been designed for people living in hospital or living at home on their own.
Our assessment is not based on a score.. We examine each individual part of the resident’s life and look at how much those aspects contribute to their risk of falling.
We know that people who are on more than four medications a day are at a higher risk of falling than people who aren't on four medications a day and that those who have had a previous fall are more likely to fall again. In those cases, we would record that information so that the next person who comes to see them will know they're at an increased risk of falling and the reason why.
How do preventative changes vary based on a person’s history and needs?
They vary quite a lot and we refer to the changes as multifactorial intervention. For some people, a lot of different factors need to be considered, whereas for others it might just be that something particular is happening at a certain time of day.
Using this GtACH program, someone may document the fact that Mrs. X is falling at 9 o'clock in the morning every day, for example, but that she doesn't fall at other times. Staff could then ask - what's happening at 9 o'clock?
Although this seems like common sense, research suggests that care home staff are so busy and staff changes so frequently, that it is possible no one has actually realized it's at 9 o'clock that Mrs X falls.
For Mrs X, monitoring techniques could then be used to find out what happens at that time of day. Her drugs may need changing or administering at different times or she may simply need new slippers because they are not fitting her feet properly when she puts them on in the morning.
Another common problem is weak muscles failing to hold the body up, which can be helped by performing routine exercises or attending exercise classes in the care home.
What we are trying to do is get the care home staff and relatives to participate in using the assessment and interventions. In cases where residents are cognitively intact and can do this themselves, staff could explain to them that if they do not drink a certain amount or walk a certain amount, that they will increase their risk of falling over.
What care home staff training is required in order to implement GtACH?
We recently carried out a feasibility study and found that the best way to train staff in using GtACH is to train them in small groups. They receive an hour's training from a fall specialist, which is presented to groups of between four and eight staff.
We then come back two weeks later to give refresher training, which is presented to big groups, where we find out how people are getting on, whether they're using the tool and what problems they may be having. Then we give people the telephone number of a fall specialist that they can ring if they have any problems.
We want to train about 80% of the staff in each care home, including everybody from the caretakers, cooks and cleaners, through to managers, so that everyone is aware of the factors that increase a resident’s risk of falling.
We also like to find somebody at the care home who can act as the main contact point regarding these issues, so that somebody is responsible in the care home for ensuring staff are carrying out assessments at the same time.
We've done two studies, one looking at ten care homes and the other at six homes, and we've never had a problem. The care home managers were always very willing for us to go in and train the staff. We use role-play to try and demonstrate how the intervention should be implemented and give staff confidence regarding actions they can take when they realise a resident is falling over.
Has GtACH reduced the number of falls in care homes?
Although very small, our study did indicate that GtACH has reduced the number of falls in the care homes that have implemented it. However, we want to do a bigger study, which we are hoping the NIHR will fund.
We are planning to use 66 care homes across the UK – 33 that would use the intervention and 33 that would not. We would then measure the outcomes across all of the care homes to see whether it reduced falls or not.
So far, the evidence is encouraging and according to the literature, the intervention is made up of all the things that reduces falls, but we'll have to wait and see whether it definitely reduces falls.
GtACH has recently won an East Midlands Innovation in Healthcare Award. What impact will this have?
It's already been amazing. We went to the prize giving last week and we've had a great deal of interest from the Academic Health Science Network. They are going to help us roll GtACH out across the East Midlands.
 We've already had one meeting with them about how to make our booklet, manual and training relevant across the whole of the East Midlands area. It's encouraged us to get our application in to do an evaluation.
We've already had one meeting with them about how to make our booklet, manual and training relevant across the whole of the East Midlands area. It's encouraged us to get our application in to do an evaluation.
We're going to use the £2,000 prize money to have our documentation redesigned so that it is a bit more suitable for the care home, rather than looking like an NHS document. Most people who work in care homes aren't nurses or therapists, so we need something that care home staff would want to pick up and use.

What feedback have you had on GtACH?
Care homes and the various different companies that own them tend to like it. They all like the idea that the training means staff are more equipped to make decisions and respond to situations themselves.
We've had positive feedback from the staff and the managers of care homes, as well as from people living in the care homes and their families, who are also able to look at the documentation and add their thoughts or tick boxes to find out what should be done.
What are your plans for the future with regards to GtACH?
We want to apply for funding to evaluate whether GtACH does actually reduce falls, which requires a large study costing around two million pounds. We are writing that application at the moment and hope to get that submitted next year.
We're also talking to the AHSM regarding other care homes in the East Midlands that may be keen to try out this new tool. We would like to go and speak to them, train them, and maybe collect some information from their care homes.
Where can readers find more information?
https://www.facebook.com/pages/FICH-Falls-in-Care-Homes/479832442084759
About Professor Pip Logan
Pip Logan is a Professor of Rehabilitation Research at the University of Nottingham and holds the first NIHR Senior non medical Clinical Academic Award. She works clinically as an occupational therapist in the community with stroke and older people patients and provides clinical input to health care of the elderly wards in an Acute Hospital.
Her main research interests are stroke, community rehabilitation, older people, falls, primary care and social Care. She has completed numerous randomised controlled trials, presents her work internationally and reviews grants for major national funding bodies.
She completed an MPhil in 1994 and PhD in 2004 at the University of Nottingham. She was awarded a National Primary Care Research Development Award (1999 -2004) and a Post Doctoral Award (2005- 2007) by the Department of Health.
She is a grant holder on a number of large research projects at present: £1.2 million to conduct an outdoor mobility study after stroke, £2 million to investigate the health care of older people in acute hospitals, £500,000 to explore rehabilitation for people after hip replacements.