Apr 24 2015
Three wavelengths will do: a practical approach for assessing the melanin and blood content of the skin was developed. It is based on a quick analysis of optical spectra.
 Many factors can change skin pigmentation, including aging, exposure to UV light, certain drugs, as well as certain diseases. A simple technique for measuring skin pigmentation could be a helpful tool for research and diagnostics. The same goes for measuring the skin blood content. Alteration of blood flow in the skin can, for example, be linked to skin irritations, inflammatory disorders, or diseases, such as psoriasis and rosacea. In addition, some systemic diseases, such as rheumatoid arthritis, atherosclerosis, and asthma, have shown to be associated with peripheral microvascular modifications.
Many factors can change skin pigmentation, including aging, exposure to UV light, certain drugs, as well as certain diseases. A simple technique for measuring skin pigmentation could be a helpful tool for research and diagnostics. The same goes for measuring the skin blood content. Alteration of blood flow in the skin can, for example, be linked to skin irritations, inflammatory disorders, or diseases, such as psoriasis and rosacea. In addition, some systemic diseases, such as rheumatoid arthritis, atherosclerosis, and asthma, have shown to be associated with peripheral microvascular modifications.
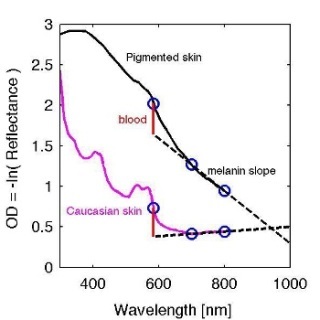
Steven L. Jacques, Oregon Health & Science University, Portland, OR/USA now presents a practical approach for assessing the melanin and blood content of the skin from total diffuse reflectance spectra. It is based on the 1985 work of Kollias and Baquer who proposed using the slope of the optical density (OD) versus wavelength, OD(λ) = –log (R(λ)), between 620 nm and 720 nm as a metric for the epidermal melanin content. Jacques’ method offers a quick spectral analysis using just three wavelengths, namely 585 nm, 700 nm, and 800 nm.
For his study, Jacques generated diffuse reflectance spectra by Monte Carlo simulations using a skin model with a pigmented epidermis, a papillary dermis and a reticular dermis. The model simulates the total diffuse reflectance that would be acquired by a camera viewing a uniformly illuminated skin site, omitting surface glare. He then derived an algorithm for predicting both epidermal melanin and papillary blood content from measurements at three wavelengths, [585 nm, λ1, λ2]. While Kollias and Baqer used λ1, λ2 equal to 620 nm, 720 nm, Jacques considered a variety of choices. He found out that almost any choice of two wavelengths in the 600–900 range could achieve the characterization of melanin. The hemoglobin oxygen saturation in the superficial mixed arterio-venous vasculature has an effect on the deduced melanin and papillary blood. This effect was investigated, suggesting some choices for λ1, λ2 that are least sensitive to oxygen saturation. 700 nm and 800 nm were used to illustrate the algorithm. The extrapolation of the melanin slope to 585 nm can serve as a baseline for subtraction from the OD (585 nm) to yield a blood perfusion score.
Jacques points out that his report is only a pilot study, and further investigations are needed. While not perfect, his quick analysis method has the advantage of simplicity and speed for assessing the blood and melanin contents in skin sites. The method may have use in patch testing of skin sensitivities to allergens and irritants, monitoring changes in blood perfusion of skin flaps, and in assessing topical skin treatments that affect skin appearance.