Pacemakers have been around for a very long time, they're great devices, critical for many people who have slow heartbeats. While they're very effective, they have some issues. There are two main aspects relating to these issues.
One is the surgical procedure to place the device. You have to make an incision in the upper chest to get the device underneath the skin. Second, in order to deliver the energy to the heart muscle there's a wire that connects this generator under the skin to the heart muscle itself.
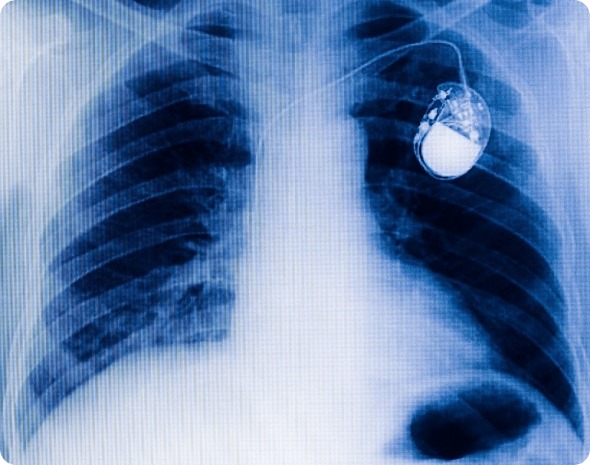
Traditional chest pacemaker one x-ray film.
There are several problems with that wire, it can fracture over time or become incorporated into the healing tissue around the wire causing scar tissue to build up.
If the wire has to be removed because of fracture or infection, removing it can be a complicated thing. Lead extraction can have some disastrous consequences. Most of the time it's okay but sometimes it's not. While the pacemaker has advanced over the past half century, we're still limited by the fact that it has a lead and a generator.
The concept for a leadless pacemaker has been around for a long time but the advances in technology have been quite recent allowing for its manufacture. All aspects, the generator, electronics and pacing element have been designed to be very small so that it can be introduced not surgically but from a transvascular perspective, through a vein in the leg into the heart and the whole device is placed within the heart itself.

The device is just over 4 cm long and 6 mm in diameter, introduced through the femoral vein attached to a flexible catheter, going up to the heart across the tricuspid valve and into the right ventricle.
The device is designed with a hook at the back end that the catheter can grab onto, which is how it is both installed and, if necessary, removed. That's basically how the leadless pacemaker works.
When was leadless pacing first developed?
The concept of leadless pacing is really old surprisingly. There was a conceptual paper back in the late 60s, early 70s. Of course that was a conceptual paper, leadless pacing was developed with the Nanostim device which was the subject of the paper we presented in 2014.
The paper focussed on the first leadless pacemaker trial in patients, which we conducted in December 2012. This was completed in Europe as a three centre study in the Czech Republic and the Netherlands, including a total of 33 patients.
The study was basically a feasibility study that a leadless pacemaker can be placed in patients, that it paces, handles appropriately out past a year. Based on that the study, the Leadless II study put this particular device in a much larger population, which is the subject of our latest presentation and paper.
The Leadless II trial was an FDA study, a total of almost 100 subjects opted in to this particular trial, in the US, Canada, and Australia. There is another device called the Micra, another leadless pacemaker made by a competitor company called Medtronic. This is also in clinical trials, but a little bit behind the Nanostim device.
How has the technology advanced in recent years?
The Nanostim is still the first leadless pacemaker. The device that was originally tested, is the exact same device that was the first in patient device.
There are definitely advancements that are ongoing though - the company is developing other leadless models that manage different Heart Rhythm needs.
Please can you outline the differences in surgical procedures involved?
With a typical pacemaker an incision is made in the upper chest to make a pocket, a space that you can put the device in and put that underneath the skin. Then there's a wire that you advance through a vein in the shoulder, you puncture the vein and advance that wire all the way to the heart.
Through the end of that wire there's a little screw and you can screw that wire into the heart tissue. This standard approach actually works quite well. At the proximal end of the wire you connect to the pacemaker and then you sew everything up. That's a traditional pacemaker.
With a leadless pacemaker, it’s all one component, which is positioned at the end of a flexible catheter. It’s introduced through a puncture in the vein in the leg and advanced to the right ventricle.
Mercy - St. Jude Medical - Animation of NanostimTM Leadless Pacemaker
The whole device is then fixed to the heart tissue similar to some traditional leads. However, unlike a traditional pacemaker, there’s no suturing. Instead just some pressure is applied at the groin puncture site.
What benefits do leadless pacemakers have over standard pacemakers?
I have to say this is somewhat theoretical in a sense that we don't have a randomized study comparing leadless versus traditional pacemakers. That'll happen in the future but the reasons we like it are a couple-fold.
First, you avoid the surgical pocket, you're not doing a surgery so there’s no risk of infection or haematoma (swelling of clotted blood) for people on blood thinners because there is just a small incision at the groin site.
The risk of infection should also be decreased because there’s no upper chest surgical incision. That's really where the biggest concern is. There is also no problem with lead extraction chronically because there is no lead, so you don’t need to worry about lead fractures or any other complications.
Also, with a traditional pacemaker the wire sits across the tricuspid valve which is a valve that separates the right atrium and the right ventricle, the top and bottom chambers on the right side, in some patients, that can cause valve dysfunction. Since this device doesn't sit across the valve that complication is pretty much gone.
There are also the cosmetic aspects. Most pacemakers now are so thin it's hard to see the pacemakers unless you really look for them, but still there's an incision and that can be an issue.
How much research has there been into the safety and efficacy of leadless pacemakers?
There has so far been the Leadless I feasibility trial, and now the Leadless II trial. This second trial is the first large prospective trial. It was not a randomized study so everybody who qualified got the leadless pacemaker.

We presented an analysis after the first 300 patients received devices and were followed for 6 months. In this analysis, what we presented were 2 data sets. We called the first dataset the primary cohort, with 300 patients followed for 6 months so we could talk about efficacy and safety in the short term and long term.
The second dataset is the total cohort after we implanted leadless pacemakers in 600 patients and are now in the follow-up phase. The total cohort includes 526 patients; we are able to study the safety data because we have implant data from all those patients.
Those represent the cohorts that we describe. The patients were the typical single chamber pacemaker patients. Their mean age is about 76 which is what you tend to find in these kinds of studies.
What adverse effects were observed in the recent Leadless II study?
The first important point is that 96% of the patients successfully received the leadless pacemaker. There were predefined safety and effectiveness end points. From those predefined end points we can see what the trial achieved.
Just over 93% of the patients did not experience adverse safety events. On the efficacy side, 90% successfully have the device and when you follow them out to 6 months all the patients are fine. These are acceptable based on current clinical studies with traditional pacemakers. Those are the major clinical end points of the study.
Just over 6% of the patients experienced some sort of safety event, probably the most important of those was cardiac tamponade. Cardiac tamponade means that at the time of implantation there was a problem with the structural integrity of the heart tissue, so blood leaked out.
This happened in about 1.5% of the patients. Tamponade is something that's been described even for traditional pacemaker implantation. This is something that's expected and we expect that this would decrease with operator experience with this type of procedure.
I want to just emphasize that there were 100 operators in this study; of those, 99 of them had never performed leadless pacemaker implantation, so it's really critical to appreciate that the learning curve is captured within this trial.
In this particular study, any complication that's been observed due to the physician's learning experience would have been captured. That's why we expect safety advances with better operator experience.
We also observed that there were 7 instances in which, for various reasons, the device had to be removed after the procedure. For example, if the patient needed to upgrade to a defibrillator.
What was nice is that in all these instances, we could take a catheter to attach to the device and remove it with the hook that’s attached to the back end. We were able to remove this device a mean of 160 days after the procedure, with 100% success rate, which was very good news.
That's great from a clinical perspective for patients that may have a problem or to replace the device with a new one. Based on how the device performed for the first 6 months, it’s possible to estimate quite accurately what the longevity of the device is going to be.
Impressively, the mean longevity of the device was 15 years. If you consider that the mean age of this population was 76, 15 years is a pretty long time. It's likely that many of these patients may not even need a second device so I think that long life speaks quite well.
What are the limitations of a leadless pacemaker? How does the reliability of leadless pacemakers compare to standard pacemakers?
First, this is a single chamber ventricular pacemaker, not a dual chamber pacemaker, which is pacing in both the top and the bottom chambers.
If you look at the frequency of single and dual chamber pacemakers being used in the world, it varies country to country but approximately 20% of the pacemakers implanted are single chamber pacemakers and the vast majority are dual chamber pacemakers, which current leadless pacemakers are currently unable to replace. That's an important limitation in terms of applicability
To have a dual chamber pacemaker requires 2 of these pacing devices, one in the bottom chamber, one in the top chamber that can communicate with each other and have reasonable battery longevity.
This is eminently feasible, the companies that make these devices are already working on the next generation dual chamber prototypes. I expect we will be testing these in patients probably within the next 3-4 years.
What do you think the future holds for leadless options for patients?
The future is very bright, once the capability for dual chamber pacemakers is realised then suddenly 100% of pacemaker patients could be affected. I think that's one of the big future advances.
There are also some other smaller issues. For example, there are some diagnostic capabilities in these leadless pacemakers that could be enhanced to make it a little closer to a traditional pacemaker. Most of that is not necessary in most patients but in some patients it can be.
There will also always be additional changes made to the devices to make them safer and easier to implant.
With regards to the regulatory aspects. This device is approved in Europe and it's in a limited market release by the company. In the US, it's not approved; my expectation is that it will be approved next year.
Medtronic is another company that has a leadless device that's in clinical studies. I think probably the best thing for patients is that it's widely talked about and most physicians know about them.
Where can readers find more information?
About Dr Reddy 
Vivek Y. Reddy, MD is Director of Cardiac Arrhythmia Services for The Mount Sinai Hospital and the Mount Sinai Health System, and The Leona M. and Harry B. Helmsley Charitable Trust Professor of Medicine in Cardiac Electrophysiology at Icahn School of Medicine at Mount Sinai.
Dr. Reddy is one of the US’ premier cardiac electrophysiologists, leading a team of physician-scientists who are developing and testing advanced therapies for cardiac arrhythmias including atrial fibrillation and ventricular tachycardias.