Enterobacteriaceae refer to the family of bacteria such as E. coli and Klebsiella that are bacterial pathogens most frequently associated with hospital-acquired infections.
Carbapenem-resistant Enterobacteriaceae (CRE) are those bacteria that have acquired genes or mutations that are resistant to many beta-lactam antibiotics, notably the carbapenem class of antimicrobial agents. Carbapenems are a class of beta-lactams, which are broad-spectrum antibiotics known to be the most effective against gram-negative infections.
%2c%20is%20a%20type%20of%20antibiotic-resistant%20bacteria.%20The%20illustration%20depicts%20the%20bacteria%20moving%20through%20the%20bloodstream%20with%20flagella-AuntSpray.jpg)
The superbug, known as Carbapenem-Resistant Enterobacteriaceae (CRE), is a type of antibiotic-resistant bacteria. The illustration depicts the bacteria moving through the bloodstream with flagella.
Resistant forms of CRE, such as as KPC (Klebsiella pneumoniaecarbapenemase) and NDM (New Delhi Metallo-beta-lactamase) produce enzymes that break down the carbapenem drugs and make them ineffective.
These bacteria are also frequently resistant to other approved classes of antimicrobials, and thus are difficult to treat because of limited options for patients. CRE infections are associated with a high mortality rate (up to 58% of patients2). The U.S. Centers for Disease Control (CDC) have designated CRE as one the three most urgent antibiotic resistant infectious disease threats3.
The dissemination of these carbapenemases in Enterobacteriaceae can be viewed as the “tipping point” for loss of beta-lactam antibiotics in modern medicine. These agents are arguably the most useful class of drugs we have for use in gram-negative infections due to their cidal mechanism of action and safety.
In view of the desire to preserve this class of antibiotics for use, we embarked on a discovery program to develop a drug that would overcome carbapenemase-mediated resistance to beta-lactam antibiotics.
That effort resulted in the discovery of new class of inhibitors that was focused on activity against carbapenemases. The first agent from our novel series of beta-lactamase inhibitors to enter into clinical development was RPX7009, currently in Phase 3 clinical trials as a fixed combination with the carbapenem meropenem.
How do Enterobacteriaceae such as E. coli become carbapenem-resistant?
Bacteria are continually adapting to their environment, developing mechanisms of resistance to the drugs designed to defeat them, and then passing on that genetic material to other bacteria.
One of the more common ways that Enterobacteriaceae become resistant to carbapenems is through the production of carbapenemase, which are enzymes that break down the carbapenem drugs and make them ineffective. These enzymes include Klebsiella pneumoniae carbapenemase (KPC), New Delhi Metallo-beta-lactamase (NDM-1), Verona Integron-Mediated Metallo-β-lactamase (VIM), and Klebsiella pneumoniae carbapenemase (IMP). KPC is among the most prevalent carbapenemases in Enterobacteriaceae in the UK4.
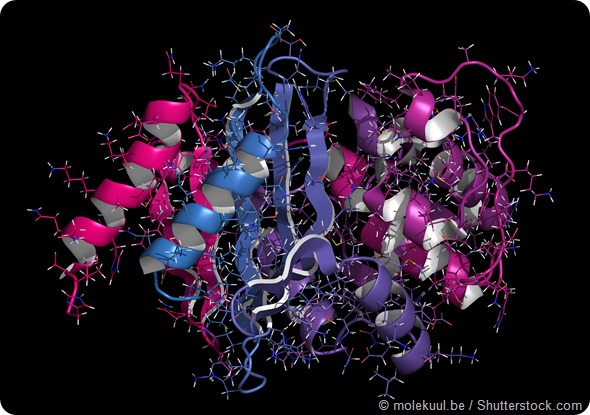
Carbapenemase carbapenem antibiotic resistance enzyme. Carbapenemase OXA-24 from the bacterium Acinetobacter baumannii. Cartoon + line model; N-to-C gradient coloring.
Who is usually affected by CRE infections?
CRE are primarily isolated from patients in acute and long-term healthcare settings, who are being treated for another condition. CRE are more likely to affect patients who have compromised immune systems, have taken long course of antibiotics, or are being treated with medical devices that can provide a pathway into the respiratory tract or bloodstream1.
Patients who are critically ill as a result of immunosuppression from chemotherapy or transplantation, surgery, or co-morbid conditions are at risk for CRE infections. CRE can cause infections when they enter the body, often through medical devices like ventilators, intravenous catheters, urinary catheters, or wounds caused by injury or surgery1.
Why don’t healthy people usually get CRE infections?
Healthy people typically don’t get infections due to gram-negative bacteria, as our host defenses are able to fight bacteria from invading normally sterile spaces. We carry Enterobacteriaceae in our gastrointestinal tract, and they are contained; however, trauma, surgical procedures, or other illnesses of the gut can result in bacteria invading sterile spaces (e.g, the peritoneum, bloodstream), and cause infection.
Healthy people can become colonized with antibiotic resistant bacteria, and thus develop drug-resistant infections in the settings and conditions described above.
How much of a public health threat are CRE infections?
CDC considers CRE to be an urgent antimicrobial resistant threat. In the U.S., the estimated number of annual cases is 9,300 and the estimated number of death is 610. However, these numbers can be misleading since they only include healthcare-associated infections caused by Klebsiella and E. coli with onset in hospitalized patients.
The case and death estimates do not include infections that occur outside of acute care hospitals (e.g. nursing homes), infections acquired in acute care hospitals but not diagnosed until after discharge, and infections caused by Enterobacteriaceae other than Klebsiella and E. coli (e.g. Enterobacter spp.)
In view of the limited treatment options in patients with these drug-resistant infections, and the high mortality and morbidity, these pathogens are of considerable concern to public health officials worldwide.
What therapy options are currently available for CRE and how well do they work?
There are no drugs approved for the treatment of infections due to CRE. Currently used antimicrobial therapies include unapproved therapies that are low, unproven effectiveness, are poorly tolerated or have serious toxicity (e.g., polymyxins).
Clinicians are faced with using combinations of drugs with unproven activity; recent data suggest that carbapenem-based regimens are associated with the best outcomes5, 6.
In developing The Medicines Company’s investigational carbapenem/beta-lactamase inhibitor combination (Carbavance® (meropenem/RPX7009)), currently in multi-national Phase 3 clinical trials, we felt it was important to obtain data on safety and efficacy in patients with CRE infections.
Our TANGO 2 trial is the first trial to be conducted with a beta-lactamase inhibitor based combination targeting patients with CRE infections. We believe these data, along with other controlled clinical trials and information in nonclinical model of infection due to CRE will provide clinicians important information should Carbavance® (meropenem/RPX7009) be successfully developed and receive regulatory approval.
What more needs to be done to build a complete picture of the incidence, prevalence, mortality and cost of resistance?
We need better surveillance networks that capture the disease burden in multiple care settings. Current systems in the US often rely on very strict definitions of infections and only survey a limited number of health care settings.
We also need more patient level data from prospective studies of new drugs where effectiveness is measured in the “real world” setting where these infections occur.
Carbapenem-resistant K. pneumoniae is becoming increasingly common in Europe. In 2012, the percentage of K. pneumonia isolates resistant to carbapenems ranged from zero (7 countries) to 60.5% (Greece).
Trend analyses for the period 2009 to 2012 showed a significantly increasing trend for the EU/EEA population weighted mean percentage, and 5 of the 24 reporting countries had significant increasing trends. None of the countries had a significant decreasing trend4.
The cost of antibiotic resistance is considerable. In 2014, the UK Prime Minister commissioned a national review on antimicrobial resistance, chaired by Sir James O’Neill. This committee’s report issued a sobering report of the economic consequences should antibiotic resistance continue unchecked to 2050, with over 10 million deaths (compared to 8.2 million for cancer).
These 10 million deaths would have an economic impact of a 2-3.5% reduction in gross domestic product, and cost the world 100 trillion US dollars4.
What do you think the future holds for CRE infections?
It would appear that we will continue to see spread of different types of CRE from different parts of the world.
While infection control and stewardship can certainly help reduce spread, the molecular genetics are very complicated and we will continue to have these infections.
It is important to remember that while inappropriate use of antibiotics augments spread of resistance, appropriate use of drugs in patients who desperately need them also results in resistance. Thus we need a steady stream of new drugs that have improved pharmacological properties and activity.
While public-private partnerships such as those in the US (e.g., BARDA) and Europe (Wellcome Trust, Innovative Medicines Initiative) are playing critical roles in supporting R&D, better economic models are needed to support industrial innovation of new antibiotics.
Where can readers find more information?
About Dr. Michael Dudley
Michael N. Dudley, PharmD, FIDSA is Senior Vice President & Head, Research & Development, and Co-Leader, Infectious Diseases Global Innovation Group, The Medicines Company, San Diego, CA.
Dr. Dudley has over 35 years of experience in all phases of anti-infective R&D in the industrial and academic setting for bacterial, viral, and fungal pathogens.
His industrial career has included leadership positions in small innovative companies involved in the discovery and development of new antimicrobial agents.
Prior to his career in industry, he held academic appointments at the University of Rhode Island College of Pharmacy, and Brown University School of Medicine where he conducted lab and clinical research and clinical infectious disease/ stewardship practice at teaching hospitals in Providence, RI.
He has published extensively on antimicrobial chemotherapy and use, served as an Editor of the journal Antimicrobial Agents and Chemotherapy, a member of the US CDC’s Antimicrobial Resistance Working Group, and co-founder of the United States Committee for Antimicrobial Susceptibility Testing (USCAST), that works closely with Europe’s EUCAST, the susceptibility testing committee for the European Medicines Agency (EMA) and other regulatory authorities.
Sources:
- Carbapenem-resistant Enterobacteriaceae in Healthcare Settings. http://www.cdc.gov/HAI/organisms/cre/.
- Munoz-Price, L. Silvia, et. al. "Clinical epidemiology of the global expansion of Klebsiella pneumoniae carbapenemases." The Lancet infectious diseases 13.9 (2013): 785-796.
- CDC Antiobiotic Resistance Threats in the United States, 2013. http://www.cdc.gov/drugresistance/pdf/ar-threats-2013-508.pdf
- Annual epidemiological report: Antimicrobial resistance and healthcare-associated infections 2014. http://ecdc.europa.eu/en/publications/Publications/antimicrobial-resistance-annual-epidemiological-report.pdf
- Tumbarello, M et. al. “Infections caused by KPC-producing Klebsiella pneumoniae: differences in therapy and mortality in a multicentre study.” J. Antimicrob Chemother doi:10.1093/jac/dkv086
- Daikos, G. et. al., “Carbapenemase-producing Klebsiella pneumoniae Bloodstream Infections: Lowering Mortality by Antibiotic Combination Schemes and the Role of Carbapenems.” Antimicrob. Agents Chemother vol. 58. (2014): 2322-2328.