Medopad is a mobile health technology company. We focus on developing software within the mobile health industry. Mobile health, from our perspective, is an industry that really was invented with the iPad.
Our vision is to create an ecosystem that connects the doctor with the patient information in the hospital, and the patient with the doctor. With that, we want to create an ecosystem of data flowing between all parties to increase efficiencies, reduce errors, and naturally, save costs. We also want to empower patients to be able to use technology in order to look after their own conditions.
From a technology point of view, in a nutshell, we believe that user adoption is key to your success in this industry, so usability and ease of use are the key words here. We feel that apps are the best way to engage with healthcare professionals because they are very busy; they don't want to learn about new technology or software. Apps usually do not come with a handbook - if they are well-designed.
Even with the best intentions, even today, if you go to a hospital with a best idea of an app, they wouldn't know what to do with you, because there's no infrastructure for that app.
What Medopad did is develop a mobile platform, which we call mHOS (mobile health operating system), that can, for example, sit behind the firewall in the hospital and connect to the different data sources in the hospital. You can then access this data seamlessly through apps on mobile devices.
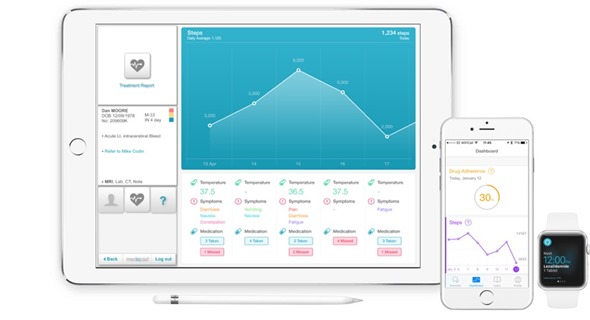
Later, with the invention of the Apple Watch, we connected the patient to this platform through a watch and a phone. Now, we have components that connect the patient to the doctor and the doctor to the patient's information in the hospital.
What impact has Medopad had on clinical practice so far?
We have developed Medopad over the past five years. For two years (2012 to 2013), we developed a back-end system with BMI Healthcare, which allowed us to certify it as a medical device, it is also FDA registered, and HIPAA-compliant as a platform.
What we did next was develop a set of universal apps, because, interestingly enough, we discovered that the challenges in healthcare are almost universal. It doesn't matter if you're in Australia or in the U.S. or in Brazil, the challenges are the same.
The first big challenge everybody started looking at was providing access to patient information. We solved this with some of our apps. What we discovered as a result was that there were significant improvements in efficiency.
Now, we are looking with the hospitals at some business cases. An early business case at one of the hospitals showed that junior doctors felt that they could save one-third of their time by using a suite of apps that we had provided to the NHS Trust. In other areas, we can see that they have more than doubled the number of patients they can see during a day using our technologies.
Our technologies are basically very simple. We are about the digital hospital – taking things from paper to a mobile device and allowing and supporting existing workflows with the technology in a very seamless way.
We are actually transitioning from paper to digital which usually means, by definition, a huge improvement in workflow, efficiency, satisfaction, a reduction on errors and a lot of other things that we are still also learning about.
What were the main challenges you had to overcome when developing Medopad?
One of the early challenges was that there wasn't an understanding of what mobile health is in the industry. We started with our idea when the iPad was invented and, at that time, people felt the iPad was a toy for children! Now, five years on, you do not see any medical publication or an exhibition where there is not an iPad somewhere on the front page!
Now, there is a far better understanding that these mobile technologies may work and do work. However, we are still a few years away from it being as widespread as smartphone usage. We take it as a given, but in healthcare, this has not happened yet.
We also have the natural challenges of cultural change. You have been using paper for the past 100 years; now you are using digital devices. The beauty is that you're using them privately, anyway so there is nothing new for you to learn. Apps are easy to use, so there is really no time wasted.
Usually the organizations we work for are larger organizations. It's not about change in one department we are working with, but the entire organization so there is also an aspect of organizational change.
How do you make sure that patient data is secure?
Patient data security was the single most important thing when we set off with the idea of Medopad. To put that into context, before we even registered our company in 2011, Dan and I researched for three months the reasons people believe that, in healthcare, patient data is at risk.
We asked why is there a mind-set that it is impossible to secure patient data and everything associated with it?
We then discovered that there are areas that really could benefit from significant improvement. The beauty of being an innovator and trailblazer in an industry, is that we start with a blank sheet, so, we have no real concerns with legacy systems. We could really leverage the latest technology, the latest platform and build a solution that is, from the architectural point of view, designed to avoid many cases of exposure of data.
In the early days, when the Cloud was a very popular topic, we believed that our clients preferred to own and maintain the patient data themselves. What we decided is that our platform should be able to fit independently behind the hospital firewall when it's connected to the hospital system, and that after we deliver it, we actually have no access to patient data anymore.
Today, we know that that is what customers want and that is why we are selling to and supplying the NHS and some other hospital groups. With that, we have already avoided a very big risk factor.
There are other approaches such as using specific multiple layers of encryption, the latest hardware encryption systems and some common-sense software solutions, that mean, for example, if the device is left somewhere, it switches itself off. We have a solution whereby if the device leaves the parameter of the hospital, it erases itself of data. Another feature we have is that the hospital's IT staff can, at any time, disable a device remotely, so you will have no access to anything.
One very important thing we asked in the early days was “Why give access to everything?" Currently, when you have a password in, let's say, a hospital, you can see everybody's patient records, historical through to future appointments. We found the doctors actually only want to see their patients’ information. We basically provided the option for doctors to see only their patients’ data, so you never have more than maybe 20 to 60 patients, at any time, by definition.
These are little steps we took on the software side to address all these issues that people felt were challenges in the area of security. Naturally, the most important thing as a result of these things we did, is to get everything certified in the early days as well. That's why, as a very first step, we had the Medopad certified and CE-approved as a medical device, which covered a lot of the security aspects as well.
In what ways do you think Medopad will affect the doctor-patient relationship?
I believe that, especially with our new product line, which we call remote patient monitoring, the relationship will be truly enhanced because of the wealth of quality data available now to the doctor and to the patient as well.
When they meet and have a conversation, they can be so precise in that conversation. The doctor will know exactly which medication the patient took on Wednesday, for example, and at what time and what symptoms they reported as a result of taking that medication. In addition, the sensors in the device let the doctor know whether, for example, the patient went for a walk that day and how that may have affected their health.
The quality of conversation is actually far higher. Also, the doctor can make a far better diagnosis and reduce error. That creates more quality time for the doctor to spend with the patient, talking about very specific information relating to that patient, especially in the chronic disease area that costs the majority of the NHS budget. I think 70% is often quoted for diabetes, cancer, and for heart disease. These areas, in particular, are the ones we want to support with our remote patient monitoring.
The idea is to open the communication lines, have more data, make better decisions and also empower the patient to look after themselves. They don't need to come to the hospital with every small question they have.
The doctor has more time; they can spend more time with patients and see more patients. Ultimately, by doing all this, the quality of care delivered will be increased.
What feedback have you had on Medopad so far?
The feedback is overwhelmingly positive.
I also have two examples that I will not forget. As innovators, our clients usually try to make our lives really hard so we can prove our technology. For example, they selected somebody who was over 75 years old, suffering from cancer and had never owned a smartphone in their life before.
We supplied the technology to the patient. Within 24 hours, she was using the technology as if she had been using this type of technology for years. Because the initial phase was defined as a trial, when we asked her to give the equipment back, she didn't want to give it back. She then kissed the watch and gave it back!
I have never seen that and for me, that was one of my key experiences. It shows you how much these technologies can empower. It gives you a sense of security when you are more in control of your own health and know that somebody on the other side also has access to your data. If you pick up the phone, they know what you're talking about, you don't need to remember what it was.
To give another example, a short while ago, one of our business development team members reported that one of our patients at another NHS Trust, who was diagnosed with cancer and going through his chemotherapy treatment, had said he had been given only a few weeks to live. He then passed on his details. He wanted to give these details to the business development team member, so that the equipment could be returned.
The next time the team member bumped into him, the patient said that the doctor noticed that on a certain day, when the patient was taking a certain medication, his movement pattern and movement went fairly low and he had reported certain symptoms. The doctor asked the patient to come in and then realized that he was allergic to one of the medications that he was prescribed for his cancer treatment. They adjusted the medication. I don't know exactly the exact status of the cancer is today, but it was basically going away as result of the treatment.
That was a result of just combining three very simple things - movement pattern with drug adherence and symptom reporting. There is no magic in it. It is not difficult, but this did not exist before. The oncology department did not have this information available and a simple correlation like that can save a human life.
Also, there are hospital CTOs that have commented on Medopad. There is a 3-minute video on our website where you'll see some comments made by independent people. This video was not produced by us as an advert and is basically just a little documentary that was made.
http://www.medopad.com/medopad_Ltd/Video_intro.html
Can you please give an overview of the cancer app you have developed?
The cancer app is a patient-monitoring app. Cancer is one of the three big chronic diseases that are perceived as big challenges to healthcare systems worldwide. It's a huge cost factor.
Statistically, in the UK, every second person will be touched by cancer at some point in their life. We felt we had to do something about it. For a long time, we were looking for a way to connect the patient to the doctor.
It was only when Apple introduced the Apple Watch that we thought: "Wow. This is a very simple interface. It's very natural, you wear it on your arm and it can be used by any age group."
We decided to try to use it to empower the patient and connect them with the doctor and the hospital. As a result, we developed and deployed the first ever healthcare app using the iPhone and the Apple Watch. It was developed with the team at King’s and launched about 9 months ago. Hospitals in West London are using it and we are also working with some of the largest hospital groups in the UK.

Many hospital groups have identified that this can be helpful to them. In particular, the private hospital groups, for example, can remotely monitor a patient that may not live in this country, but who comes to the UK for their treatment. They have been trialing the solution in order to remotely monitor their patients.
In what ways do you plan to develop Medopad moving forwards?
Medopad is all about data. By creating this ecosystem, we want to add value wherever we can within the healthcare industry. Healthcare also covers the insurance industry and the patients themselves. Naturally, we started with healthcare, in terms of hospitals, and healthcare providers.
We want to create an ecosystem that really brings value, and, ultimately, in 3, 4, 5 years, we want to use our ecosystem of data to create a more intelligent and deeper understanding. Learning from that data can then, for the very first time, help our clients, the patient, hospital, insurers, to increase their efficiency, save costs, and improve care outcomes. It's all about big data – IoT in the future.
Today, we feel the biggest value we bring by empowering the patient to look after themselves and by bringing efficiencies to our care providers, is in helping to reduce errors, reduce costs, empower better care and, for example, in the case of the NHS, helping with the NHS digital hospital strategy.
We are also partners of IBM, Intel and we work closely with other organizations as well to deliver our solution. This is not something one company can deliver. We do that together with others, to basically enhance our offering to our end-users and clients.
What do you think the future holds for mobile health and how do Medopad plan to add value?
I think mobile health is still in its early days. It’s not about the future of mobile health, but about the fact that the future is mobile health.
We are using these powerful devices on a daily basis; they are in our pocket and we are wearing them. The future is all about using mobility in healthcare to provide better care to improve efficiencies and reduce the errors.
From my perspective, it's a ‘no-brainer’. It costs next to nothing, there is hardly anything to learn, more and more innovation on the hardware side can talk – software and hardware can seamlessly integrate. We can connect and help people collaborate, communicate and share all these things and improve care.
It's also the simplest and fastest way for people to save money. By definition, mobile health is very mobile, very accessible, the apps don't cost very much and in many cases, we already own the hardware.
Also, it’s global, which is very important. Again, the problems we have here and the problems Medopad solves with its innovation are the same problems experienced in China, in Canada and in Chile, for example. The beauty is that when we solve it here in the UK, we can transfer the solution. We just need to locally adapt the language and so on, so we can provide solutions to them.
Ideally, we will maybe one day connect the people in Chile with the people in China. We may have doctors in the UK give second opinions to the doctors in the UAE, so that patients don't need to even travel that much for their treatment, and, again, increase the likelihood of them improving and basically becoming better sooner.
In this context, I should mention that Medopad was awarded the 2014 best medical app by MEDICA, the largest healthcare event worldwide. Last year, Medopad was also voted the most innovative company in the UK. The company has also won a wide range of awards, from MIT to Oxford.
I think there is also a better understanding now from the outside world, of the value our industry's trying to apply, but, no doubt, there are still a few years ahead of us that might prove challenging. However, I think in 5, 6, 7 and a maximum of 10 years, people will probably say: "What is so special about using my phone to manage my condition?"
KPMG wrote an article about Medopad and the value of the worldwide challenges we are addressing. They really see this industry and what we do as something that's wildfire. It is something everybody needs and it doesn't cost very much, so it’s common sense. It works, it's proven, it's secure and everybody is a winner using mobile technology… specifically, our technologies on our ecosystem.
KPMG described us as a ‘unicorn’, which means the companies potential of achieving a $1 billion valuation. We are one of the fastest growing health tech companies, based on our valuation.
The company's valuation is no secret. It shows how the industry is perceived out there, how the financial markets value or see this industry growing, and how much potential they actually see in it.
We have some amazing investors on-board, including Bupa and Bayer Pharmaceutical which were some of our earliest investors. There are some really amazing individuals as well.
Where can readers find more information?
About Dr Rich Khatib, CEO
Drives company strategy, operations and finance. His career in EMEA & US, include CEO of a $1B impact investment foundation of the Oceanic Bank International.
Previously he kick-started Mondus, a leading European electronic procurement firm, as vice president and 1st team member.
In 2001 Mondus sold to Telecom Italia for a total deal of €400 million, delivering a 10X return on the original investment of VC firm 3i.
He studied business in Germany and holds a DPhil majoring in economics from Oxford University.
About Dan Vahdat, CTO
Drives product vision, technology and strategy. He is an award winning innovator in the fields of science and technology.
Dan’s professional career spans from IT to medical technology including two years at Johns Hopkins in the US.
He studied Engineering and Mathematics, after which he pursued his PhD in Bio-Engineering at Johns Hopkins and Oxford University.