The best example is in aviation, which has been the primary mission of our parent company CAE Inc. The first mandatory courses in civil aviation, known as Cockpit Resource Management or CRM, were implemented decades ago.
Most of us don’t remember a time when pilots and crews learned to fly without simulation. We can’t imagine taking a flight with a crew that is flying for the first time and has only theoretical knowledge of the cockpit and the plane.
In healthcare, we have physicians, nurses and paramedics who know the textbook by heart and know exactly what they need to do, but have never experienced the procedure first-hand, or they have no experience responding to adverse events that may occur.

Simulating a code blue adverse event with CAE healthcare’s iStan simulator. Courtesy of CAE Healthcare.
Currently though, this is how healthcare professionals are taught, first theoretically, then directly on patients under supervision of more experienced healthcare workers.
What do you think simulation best teaches students that can’t be learnt with theoretical learning?
Communication is one of the key skills that simulation teaches in a live scenario with multiple learners interacting. For example, if you're in an operating room with open-heart surgery and 10 people gravitating around the patient, you need to properly communicate.

Simulation training at USC Keck School of Medicine. Courtesy of CAE Healthcare.
You need to have some kind of situational governance. Both the anesthesiologist and the surgeon may be doing the right thing, but if they don't properly communicate they may be going in different directions.
In healthcare, we need to learn how to interact and work in a team environment, and that's key. We’ve been putting a lot of effort around that. We see teams of professionals around patient simulators, fully immersed. Nobody takes a step back to challenge the realism of the experience. They're completely into it. That's the goal. That's how they're going to learn.
What is being done to increase realism in the physical simulators? How complicated can they feasibly become? Do they have pain sensors/emotions/underlying conditions?
We're transferring best practices and technologies from our full flight simulators to our healthcare simulators. Right now the technology is rapidly evolving. For example, because of the miniaturization of processors in smartphones, we have been able to make our simulators more and more intelligent. In the future, there are endless possibilities to what we could do to increase realism.

Demonstration of the internal complexity of CAE healthcare simulators. Courtesy of CAE Healthcare.
We can already simulate giving medication to our simulated patients, and because they have integrated physiology, they're going to react accordingly, like live patients.
What does CAE Healthcare offer in the simulated medical teaching industry? What does makes CAE Healthcare unique?
CAE Healthcare is the most innovative player in the field of healthcare simulation. Innovation is in our DNA. The breadth of our portfolio in high-fidelity simulation also makes CAE Healthcare unique.
CAE Healthcare is a leading provider of high-fidelity patient simulators, interventional/surgical simulators and medical imaging simulators, mostly for ultrasound. We also offer the most realistic phantoms, models on which you can practice ultrasound-guided procedures.

CAE Healthcare’s latest ultrasound simulators, the Vimedix. Courtesy of CAE Healthcare.
CAE Healthcare is also the leader in audiovisual and center management solutions, which are like the central nervous system of a simulation center. They are used to coordinate scheduling, performance assessment and everything that's going to be useful for debriefing.
Finally, we have the educational content for the simulators. We're not just selling hardware. We're selling a solution. What’s exceptional about our simulators is that they come with the right content and that added layer of knowledge comes from our Academy.
We're unique because we have 20 full-time clinicians and instructors working full-time for the company. I'm a cardiologist by trade, I used to be an instructor and university professor. We also have a network of adjunct faculty that provide content and allow us to offer services.
Our solutions range from consultancy to staffing training centers to designing and building training centers, exactly what CAE does in aviation. We have the largest portfolio in the healthcare simulation industry, and because we offer all these segments, it makes a difference in our potential solutions. We create physiology-driven patient simulators. Our platforms are driven by sophisticated models that emulate physiology. There’s no other company doing that in our field.
When you perform an intervention on a patient simulator or a surgical platform, the simulator will adapt just like a patient would. The instructor doesn't have to change the vital signs or physiology as they go. It's automatic, and the simulator models the reactions of a normal patient.
What applications have CAE products been used for?
We're a global company, with a presence in 120 countries, and we're leveraging the network of CAE Inc.
We cover a range of specialties. We sell both to the civilian and the military markets. We cover EMS, trauma and military as well as nursing and medicine.
We supply patient simulators to medical schools, but we also provide interventional simulators and ultrasound simulators, which are more tailored to physicians and healthcare providers.
What features are used to convey realism in the simulators?
We have a number of features that bring about realism. For us, the most important aspect of realism is to make sure that the platforms are going to fulfill the training needs.
That's where we put our focus. Our simulators have to accurately respond as human beings would during the intervention. It’s a key differentiator for us on all different types of platforms. For example, our virtual reality interventional simulators are haptic-enabled which means that they provide force feedback and make the procedures more realistic.
We’ve been taking ideas from the civil aviation side of CAE Inc. where they have strong capabilities in terms of visual effects of simulation. This is one of the technologies we're translating to healthcare
The visual technology inspired our virtual reality ultrasound, which is very realistic. Ultrasound is unique in comparison to other imaging methodologies. Unlike CT or MRI scanning where the machine produces the images, ultrasound is completely operator-dependent.
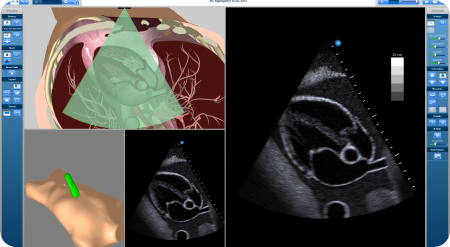
Screenshot of the software actively simulating the real time movement of the trainee. Courtesy of CAE Healthcare.
If you do an echo exam of the heart, you need to be exactly between 2 ribs, avoiding all the shadows and artifacts of the lungs and ribs to capture the right image. Deviate a few degrees or millimeters to the left or right and you miss the image. In our simulator, the manipulation and tracking of the ultrasound probe is extremely accurate. That's key to acquiring the skills that are central to proper ultrasound scanning.
In every segment of our business, we put significant energy and resources to making our products as realistic as possible. CAE Inc., in all its segments has achieved this kind of high fidelity. One of our key goals is to maintain the reputation of being a high fidelity powerhouse.
After each training simulation with physical simulators, how easy is it to replace the constituent parts, the skin and organs that have been cut and operated upon? How long is the lifetime of each of the products before parts are replaced?
Most of them are incredibly robust. The Blue Phantom models, for example, are marketed for their durability. They have a patented tissue technology that withstands thousands of needle punctures without creating any holes or hints for the following students.

Blue Phantom injection and ultrasounds simulator. Courtesy of CAE Healthcare.
Obviously, procedures that involve cutting will need repairing and replacing after a time. We offer products for procedures like cannulation or practicing injection, which have an incredible lifespan and can be used multiple times.
Customers who purchased from us maybe 12, 13 years ago are still using that same equipment. Those machines are still going. We're quite proud of that. A few of our early simulators with a serial number in the single digits are still around, and still working.
What limitations are there in simulated teaching? What can’t be simulated? Do you think this scenarios will be overcome in the future?
Right now, we have the technology to generate extremely realistic scenarios, so the question becomes "what is educationally needed?" We could create mannequins and interventions or scenarios that look more realistic, but it's not a decision of the company. That is a discussion that we have with our customers and the experts.
What we aim for is fulfilling the educational need, and we achieve that. I have seen simulation scenarios where the students cry at the end because they lost the patient.
The patient is plastic and pixels, but they feel as though they lost a patient. We have achieved the suspension of disbelief, which is our goal. We want really to transport the learners into the exact stresses they would experience with a patient, with the adrenaline rush that makes it very difficult to think properly and very difficult to act properly if the next step is not a reflex.
This experiential learning is all about creating reflexes and muscle memory in preparation for real and catastrophic occurrences when they will need to think fast. We achieve that with the suspension of disbelief.
We currently have technology that's more than sufficient to achieve that suspension of disbelief. The students are really immersed into it, and that's a great accomplishment.
What does the future hold for simulated medical teaching and simulation models? What does the future hold for CAE healthcare?
Right now, we're in the early adoption phase for simulation in healthcare, in contrary to other high-stakes environments where simulation is mandatory. If you look at nuclear plants, aviation, or the military, they all adopted simulation decades ago.
Healthcare has been trailing behind for a number of reasons, but I think the catch-up phase has already begun. We're on the steep part of the slope as we start to realize the impact of preventable harm from medical errors.
The latest research suggests that close to half a million US patients die every year due to preventable harm. This makes medical errors the third leading cause of mortality.
Now that we know that, and we have the knowledge to improve these numbers, we're at the tipping point where there's a consensus that we should adopt simulation to better prepare.
Simulation is not only about simulators. As I said, it's training. Simulators are an instrument, part of a more global approach. That includes a shift in culture, including the high-reliability organization principles that other industries have adopted. The checklist. Proper communication. Mandatory, regular recertification. You don't necessarily need a simulator for all of that all the time, but it's part of this culture of minimizing risk and optimizing safety in a healthcare environment.
Where can readers find more information?
caehealthcare.com
About Robert Amyot
Dr. Robert Amyot was appointed President, CAE Healthcare in April 2014. Dr. Amyot was previously CAE Healthcare’s Vice President for Medical Programs and Chief Medical Officer, a position he held since January 2012. For two years prior to that, he served as Director of Ultrasound Education for CAE.
In 2006, Dr. Amyot initiated the Vimedix project and is the inventor of the first simulator for transthoracic echocardiography to incorporate virtual reality technology. He cofounded VIMEDIX Virtual Medical Imaging Training Systems, which was acquired by CAE Healthcare in January of 2010. The CAE Vimedix ultrasound simulator is now used in leading medical centers around the world, including the Mayo Clinic, Beth Israel Deaconess Medical Center and Massachusetts General Hospital.
A cardiologist-echocardiographer, Dr. Amyot graduated from University of Montreal in 1992 with a degree in medicine. He completed his residency at the University of Montreal, and subsequently gained fellowship from the Royal College of Physicians and Surgeons of Canada in internal medicine in 1995 and in cardiology in 1996. In 2007, he was promoted to associate professor of medicine at the University of Montreal. He has published more than 60 book chapters, abstracts and articles, and has been involved as an investigator in more than 30 clinical trials, mostly in the field of echocardiography.