The main challenges for lower limb amputees are safety and pain. Lack of sensory feedback leading to an increased risk of falling, compensatory movements due to instability causing lower back pain and discomfort between the residual limb and prosthesis all contribute to a significant reduction in confidence and an inability to live a full life.
For 40 years we have been applying the latest engineering and advances in technology to restore the function of the knee and ankle/foot in a modular prosthesis. This resulted in the first use of composites for a lighter limb, the first application of multi-axial ankles to reduce the physiological cost of walking, and microprocessor-controlled knees to accommodate variations in walking speed. We made rapid progress with the creation of hydraulic ankles that adapt to different terrain and uneven ground, providing feedback to the amputee through the interface of prosthesis and their stump.
We reached the point that the underlying science of locomotion enabled us to mimic the natural ankle/foot relationship with the knee and identify how these joints needed to coordinate and work in synergy. This would provide greater stability, greater comfort through the re-distribution of loads at the interface, while requiring less energy, for example when walking faster, going down ramps, standing still, or standing on slopes. Amputees were able to load both limbs more equally, reduce compensatory movements and subsequent risk to their musculoskeletal system.
It was then a natural step to develop an integrated prosthesis where the knee and ankle/foot operate in a proactively coordinated manner, working in more natural harmony and able to meet almost any situation in which a prosthesis wearer might find themselves. This was the birth of integrated prosthesis.
How does the intelligent prosthetic limb work? How does the system adapt automatically to different conditions?
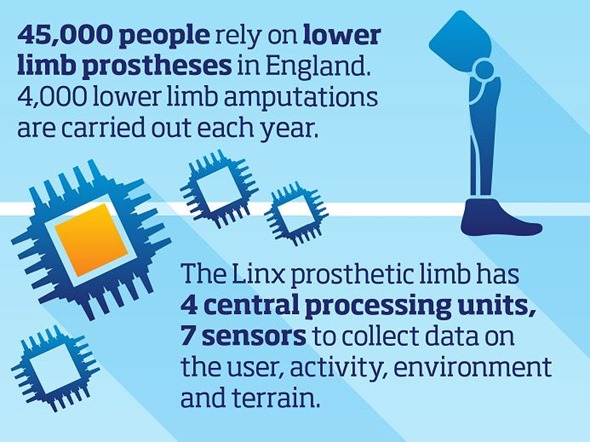
The new next-generation Intelligent Prosthesis is an integrated system, which combines the ankle, foot and knee in one structure and houses an array of sensors and hydraulic and pneumatic damping actuators linked with composite and pneumatic springs. These harvest natural, human energy and return them at the correct instance under the control of four microprocessors.
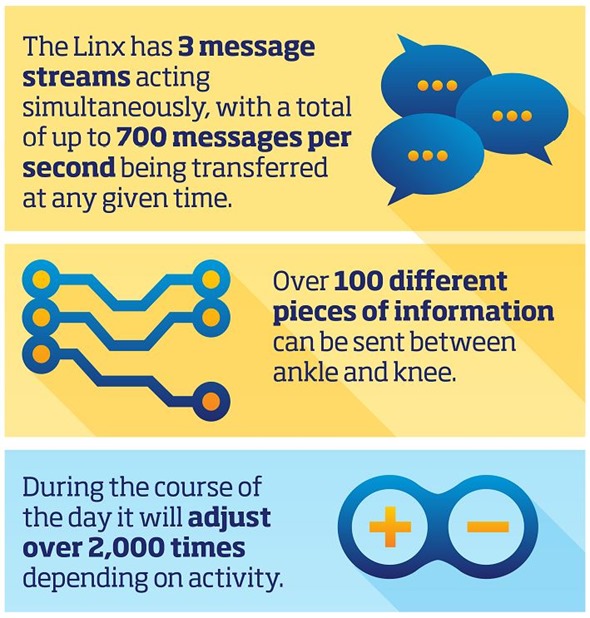
For example, the sensors in the foot will detect a slope and instruct the knee damping to increase, or when amputee comes to a stop, the sensors in the knee detect this, re-confirm with the ankle, and increase the resistance settings of the joints to increase to offer a natural and comfortable standing configuration, tailored to the individual.
The intelligence is hidden in the limb to provide a seamless operation, based on the limb’s awareness of the external environment, internal loads and motion generated by the amputee. The prosthesis adapts to offer an optimum function and the least compensatory action by the user. Amputees have commented that they do not always need to think about walking, standing, sitting, going down stairs or navigating a ramp. In fact, they are sometimes surprised to find they are not even aware the ground has changed, unless it was something they saw for themselves.

What were the main challenges in developing the Linx Limb system and how long did it take?
The main challenges were to establish a base or a platform that we could experiment on and establish the link between the knee and ankle, then identify the hardware requirements, and finally package them in a space that was practical, visually appealing, and light enough for the wearer to experience the benefits.
Today, the normal expectation is for battery-operated devices to last several days. The battery technology we have needed to be customised, tested and certified, before being packaged so that the mass centre of the limb is nearer to the knee reducing any abnormal pull forces on the stump socket. These are just a few examples: we had to integrate the entire R&D team around Linx which was very exciting to watch, almost like a dance, and see how solutions manifested one by one.
The project took three years from the application for patents, developing a prototype, structural, functional and EMC testing, and trailing on amputees, until freezing the design in 2014 and starting an early adopter programme just before the New Year. Watching user reactions was the next exciting phase.
What feedback have you had so far?
Keeping everything crossed, it has been very positive so far. Immediate feedback included the ability to safely go over an obstacle, or not having to think about them so much, adapting to the ground, compliance of the limb going over the edge of the road, standing and relaxing for the first time.
In one case, doctors decided to delay an amputee’s treatment of their opposite knee and lower back pain: after a few weeks of using Linx, it was no longer a major issue. Linx is offering extra comfort, the confidence and ability to stand up upright and be balanced in almost all situations and to safely sit down. In the case of a few bilateral amputees, we are now learning how to make the right leg ‘talk’ to the left leg, as all the hardware and software are already in place.
In another case, we were terrified but thrilled to watch an amputee walking backward down a slope, as Linx did what it was supposed to do.

How long does the Linx take to calibrate to the way its wearer naturally walks? How often is calibration required?
The interaction of the user interface software and internal Linx firmware take care of this - the calibration is mostly automatic and works by measuring the way the individual amputee walks. For able-bodied people, when you look at the biometric data of forces and the motion of joints and segments, walking is like a signature.
With amputees, each residual limb is of a different length, different strength and different design of interface to the prostheses. This means the customisation is even more critical and complex, and needs to be matched to individual ability, power and control.
The programming takes around 10-15 minutes. The amputee is first set with values when standing still, then sitting and then standing up. The limb learns from the natural motion. The Prosthetist can then fine-tune the setting based on feedback. The amputee then walks for about 10 steps and the system learns most of what is needed for calculating the setting required for that individual.
There are further advanced settings where the amputee goes on a ramp, or on the stairs, or walks at different speeds - pre-calculated values are further tuned to match the user in those environments and how they meet the differences in terrain.
Where is the Linx currently available? Is it covered by the NHS in the UK?
The Linx has been available globally for over a year. Most of its uptake has been in the USA and Germany. The UK currently has the 3rd largest uptake, mainly in Scotland as NHS in Scotland has allocated funding.
In England the NHS has not as yet fully addressed the need for the advanced technology and the few fittings of Linx have been through special funding. The private sector in the UK is beginning to use this technology more.
We hope through increasing awareness of the benefits and by making a long-term health-economic case that the lowering of the overall cost of care for amputees in their life time can be calculated, we can convince the authorities of the need for this early investment and accelerate access to the technology. The benefit of technology takes time to be understood and broad-reaching advocacy is needed.
What advances does Blatchford plan to make to the Linx moving forwards?
In 2010 we were finalists for the Royal Academy of Engineering’s MacRobert award for development of the first commercial biomimetic hydraulic ankle. Our R&D team was recognised amongst the top ten most innovative in the UK. That recognition, combined with the legacy of the 2012 Paralympics acted as a catalyst for the creation of Linx which is this year’s MacRobert award winner, competing against a new MRI scanner from Siemens and new engine from Jaguar-Land Rover.
As the award is renowned for spotting the ‘next big thing’ in technology and having been through its selection process (the most comprehensive in the UK engineering sector), this acknowledgement of our capability has given us the courage to take even greater steps by mapping out Linx for less active users (which are the majority of amputees) to enable them to safely sit and stand.
It is hoped this will reduce the level of care needed for elderly amputees and provide prolonged independent living. After that, external power for prostheses, to help replace the energy generated by the original limb is an ultimate goal.
What do you think the future holds for intelligent prosthetics?
This is the beginning of integration. In the next 20 years I think all limbs will be integrated as already happening in upper limb, while sensors connected to the body will control the limb. In the next 5 years, advances will be in the software that controls the limb.
We have begun to better understand the natural coordination of lower limb joints and segments and that is opening new exciting opportunities for design. The sensors can predict and enable the seamless activity of limbs whether the user is doing weight lifting, taking a shower, or changing to a dress shoe.
Where can readers find more information?
The Linx and Blatchford websites have detailed information: https://www.blatchfordmobility.com/en-us/products/limb-systems/linx/ and https://www.blatchfordmobility.com/en-gb/
For more information on the Royal Academy of Engineering’s MacRobert award: www.raeng.org.uk/prizes/macrobert

About Professor Saeed Zahedi
 Professor Saeed Zahedi OBE FREng RDI FIMechE PhD: with over three decades of leadership in international prosthetic innovation, accolades include: Fellow of the Royal Academy of Engineering and Institute of Mechanical Engineers, visiting Professor, Royal Designer for Industry, Vice Chair of ISPO UK, member of ISO, CEN and IEC Working Groups in medical robotics, orthotics and prosthetics, prize winning author of over 125 scientific publications, 35 patents, Special Commendation in the 2011 Prince Philip Designer prize, BHTA Life Time Achievement award in 2013.
Professor Saeed Zahedi OBE FREng RDI FIMechE PhD: with over three decades of leadership in international prosthetic innovation, accolades include: Fellow of the Royal Academy of Engineering and Institute of Mechanical Engineers, visiting Professor, Royal Designer for Industry, Vice Chair of ISPO UK, member of ISO, CEN and IEC Working Groups in medical robotics, orthotics and prosthetics, prize winning author of over 125 scientific publications, 35 patents, Special Commendation in the 2011 Prince Philip Designer prize, BHTA Life Time Achievement award in 2013.
He was responsible for the commercialisation of the first Intelligent Prosthesis in the early 90’s and in 2012 led the team for the development of the first Integrated Biomimetic lower limb Prosthesis for lower limb amputees utilising microprocessor-controlled ankle/foot and knee joints acting in synergy resulting in increased efficiency and independent living. This commercial product, the Linx, won the BHTA innovation award in 2015 and won the Royal Academy of Engineering’s MacRobert award in 2016. His current work with his team is on the development of the next generation of customised prostheses and orthoses aimed at the future integration of products and services, targeting affordability and access using additive manufacturing, aiming at increased efficiency and prolonging independent living.