Cancer remains a leading cause of death worldwide, and the global cancer burden is expected to increase by 70 percent over the next two decades.
In spite of these statistics, there is still much to celebrate in the progress we have made in the fight against cancer. In the past five years alone, 70 new oncology therapies have launched, and there are countless other pipeline agents in development that show promise for improving patient outcomes.
While there continues to be great value in progressing the development of new therapies, success here does not happen quickly. The highly complex and risky process can take well over a decade. Not only that, but as few as 1 in 5,000 compounds tested actually reach patients.
Because of this, it is important to also invest in the wider utilization of existing, approved therapies while this new exploration is underway.
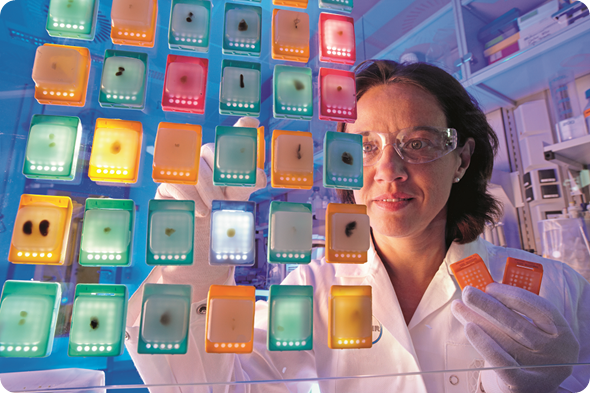
Researcher inspecting tissue samples
How can we maximize the clinical utility of existing therapies?
The knowledge our industry has amassed on cancer has readied us to address its mounting burden. We have long known that cancer is not a single disease, but over 100 different diseases. However, there are patterns in the way it forms and grows which hint at the way certain therapies may perform in certain areas of disease.
At Bayer, we have continued to study our existing therapies to expand our understanding of their clinical use across different tumor types, so that we can extend these treatments to additional patients that may derive benefit.
Why do certain cancer types and tumor micro-environments behave in similar ways?
Through industry research, we have come to understand the commonalities among various types and subtypes of cancer, along with the underlying mechanisms of cancer initiation and progression that exist when key molecular signaling proteins and pathways are mutated or activated.
The same cellular processes that play a critical role in the modulation and angiogenesis of healthy cells can malfunction and spur the growth of cancer cells that keep dividing in an uncontrolled fashion until tumors form. Then, signaling pathways within the surrounding tumor create new blood vessels, which bring the tumor oxygen and nutrients and fuel survival.
Because these processes are replicated across different areas of the body, both in normal cell growth and cancer cell growth, we can reasonably predict where a given targeted therapy or other treatment modality may work in multiple tumor types.

Researcher conducting genome analysis
Can you please give some examples of commonalities amongst cancers?
One common pattern we see in cancer is the overexpression of proteins. For example, mesothelin is a protein that is overexpressed in many solid tumors, including mesothelioma as well as pancreatic and ovarian cancers.
In other settings, like in hepatocellular carcinoma and colorectal cancer, mutated growth factors can attach to tyrosine kinase growth receptors, causing the signaling pathway within the cell to over-activate and produce cancer cells.
There are also commonalities in how certain types of cancers advance and metastasize, or spread, to other areas of the body. We have learned that breast and prostate cancers, among others, typically metastasize to the bone in advanced stages, and so are conducting research to understand whether the same bone targeting agents that have a proven survival benefit in one tumor type can be replicated to others.
What research is needed to discover new ways to utilize existing therapies?
There are several clinical studies underway across the industry which are evaluating existing therapies in new tumor types.
Also, efforts are ongoing to collect real-world clinical outcomes data to help identify existing, effective treatments for cancers based on their genomic profiles. Bayer has recently joined one such effort – ASCO’s Targeted Agent and Profiling Utilization Registry (TAPUR) study, its first-ever clinical trial.
The TAPUR study is a non-randomized clinical trial that aims to describe the performance – both safety and efficacy – of commercially available, targeted anticancer drugs prescribed for the treatment of patients in a range of cancer types with a genomic variation thought to be a drug target.
Is this something Bayer is focusing on at the moment?
Yes, this is an area that Bayer has been focused on for some time now. Perhaps the best and most recent example of Bayer’s efforts in this area is our RESORCE study. In this study, a targeted therapy from Bayer which is already approved for certain stages of colorectal cancer and gastrointestinal stromal tumors showed a statistically significant improvement in overall survival in patients with unresectable hepatocellular carcinoma (HCC) who progressed during treatment with sorafenib.

Biobank with frozen samples
How important is the exploration of predictive or prognostic biomarkers in identifying patterns of disease?
Biomarkers make it possible to detect and classify pathological processes, monitor the course of therapy and help provide early indications on how likely side effects are to occur or how likely an individual patient is to respond to a particular treatment.
In some cases, biomarkers may be prognostic, and define the affects a tumor will have on patient outcome, or predictive, and define the effect of a treatment on the tumor.
Ultimately, biomarkers may help tailor medicine to patients with particular characteristics – an underlying approach to targeting the right patients with the right treatment at the right time.
What do you think the future holds for expanding the potential of existing cancer therapies?
Bayer, like many others, is investigating patterns in how the immune system is activated in fighting cancer, through the exploration of existing and novel immuno-oncology agents.
In addition to the oncology research that is advancing our understanding of the patterns of cancer, there are a number of projects, like The Cancer Genome Atlas, which are synthesizing genomic data and creating molecular tumor maps with unprecedented precision and detail.
With projects like these and Vice President Joe Biden’s announcement during ASCO about the public release of the National Cancer Institute’s Genomic Data Commons, we are in a better position than ever before to identify the ‘core’ cancer genes and pathways that will broaden treatment options for patients in need – both those that are novel and those that are already proven in other cancer types.
With this understanding, there is an incredible opportunity to expand the clinical benefit of existing cancer therapies. In particular, with better companion diagnostics, we will also be able to better stratify patients according to particular characteristics to potentially further improve patient outcomes, while minimizing treatment complications and side effects.
What’s Bayer’s vision with regards to exploration of current cancer therapies?
At Bayer, we are advancing one of the industry’s most diverse oncology portfolios, with a mix of targeted therapies, radiopharmaceuticals and other treatment approaches that can offer meaningful progress to doctors and patients battling the toughest cancers with high unmet medical needs.
As we progress the development of novel approaches to cancer treatment at Bayer, which include immuno-oncology, antibody drug conjugates and targeted thorium conjugates, among others, we are also prioritizing extending our existing treatments to additional patients that may derive benefit.
Where can readers find more information?
To find our more information about Bayer’s research focus in oncology, readers can visit http://pharma.bayer.com/en/innovation-partnering/research-focus/oncology/.
About Dr Mark Rutstein
Mark Rutstein currently holds the position of Vice President, Group Head, Global Clinical Development Therapeutic Area Oncology at Bayer where he oversees the clinical development strategy of several oncology therapeutic kinase inhibitors.
Prior to joining Bayer in February 2013, Mark was the Associate Vice President for Oncology Clinical Development at ImClone Systems where he led the clinical development of anti-angiogenic and anti-lymphangiogenic oncology therapeutic agents. Previously, he was a Clinical Research Director at Amgen where he contributed to the global regulatory approval of a novel hematologic agent.
Mark received a medical degree from the University of Massachusetts Medical School in 1999, completed an internal medical residency at Brigham and Women’s Hospital in Boston in 2002, and received a master of business administration from Cornell University in 2004. A board certified medical internist, Mark worked as a hospital based medical internist prior to joining the pharmaceutical industry in 2004.