Stroke is the epidemic disease of the twenty-first century and the second most frequent cause of death in 2011, accounting for 11% of all deaths worldwide. Stroke is also the second most important cause of permanent disability and one in five women and one in six men suffer a stroke.
Similar to myocardial infarction in acute ischaemic strokes clots are blocking arteries in the brain, resulting in tissue damage with consecutive neurological deficits or even death, if the artery is not reopened immediately. Therefore, the main aim of acute stroke treatment is the reopening of the blocked arteries.
The impact of stroke is tremendous, in terms of the personal fate of these patients and their families, but also the whole society. For example, if a young person suffers from a stroke they are no longer able to go back to work when the outcome of the stroke is poor. This impacts society as a whole as well as healthcare and has incredible socio-economic consequences. It’s very important to appreciate the impact of stroke all over the world.
How has stroke treatment changed over the last couple of decades?
The success in acute stroke treatment started 20 years ago, when there was no effective and evidence based treatment against stroke. In 1995, the first trial showed that intravenous thrombolysis with IV rt-PA is significantly better compared to placebo in patients with an acute ischaemic stroke.
It was called the NINDS trial and this was the first major breakthrough in acute stroke treatment. This therapy significantly improved the outcome of many stroke patients all over the world.
Even though this drug is better than placebo, many patients couldn't be treated because of the narrow time window as this therapy is effective only when provided within the first 4.5 hours after symptom onset.
This is because intravenous thrombolysis is very effective in the very early hours and its effect then begins to decrease rapidly. This presents a major challenge, treating patients within this short time frame, especially for patients living in rural areas or in patients, waking up with a stroke.
A second problem is that patients with occlusions of large vessels and with large clots did not undergo recanalization sufficiently following IV-tPA. Therefore, new treatment approaches had to be investigated to reopen these blocked arteries. One possibility were endovascular procedures, which means going into the brain with a catheter and trying to remove the clot (similar procedure as in patients with myocardial infarction).
There are several devices which have been specifically designed for this type of procedure. First generation devices were able to reopen the occluded arteries, but large studies did not show any benefit of these devices compared to the treatment with IV-tPA. however.
After 2006, new devices – so called stent retrievers - were introduced. These devices open the blocked arteries by squeezing the clot into the meshes of the stent. These stents with the clots are then retrieved out of the arteries in order to restore blood flow of the vessel again.
The use of stent retrievers has recently been studied in many different trials, to date there are six published, large, randomized, controlled trials and one more that is to be published soon. All seven trials showed that the combination of the drug (intravenous thrombolysis) and the device is significantly better than intravenous thrombolysis alone, increasing the number of patients which survived without major handicap after endovascular therapy.
However, endovascular therapy with and without intravenous thrombolysis is only possible for patients with an acute occlusion of major vessels, whereas intravenous thrombolysis alone remains the preferred treatment for patients with occlusions of smaller vessels, inaccessible for catheters.
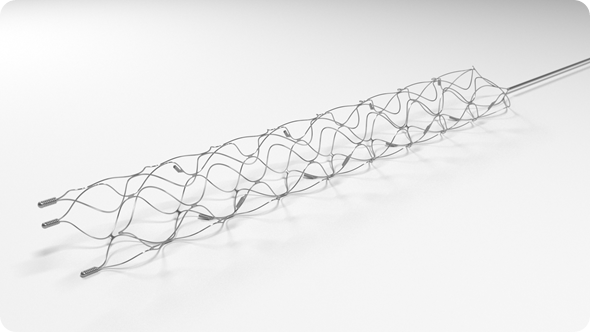
Stent retriever devices used in mechanical thrombectomy. Image credit: Medtronic
Catheter based therapy is an incredible breakthrough in acute stroke treatment as the number of patients needed to be treated to reduce a major handicap or death is now 2.6. I'm fairly sure that this will be responsible for saving many lives and handicaps in the near future.
In what ways does stroke treatment currently differ across countries in Europe?
There are vast differences in stroke treatment across Europe, which is a major problem. Intravenous thrombolysis is now available in many countries, however there are still large contrasts between Eastern European countries compared to some Western European countries.
When it comes to endovascular therapy, a lot of countries are not yet prepared for the most recent major breakthrough in treatment. Even though we now have the most efficient therapy for acute treatment ever it’s not available for patients in many areas because hospitals are not properly equipped to deal with such procedures, which requires trained neurointerventionalists and Angio suites.
Currently we are assembling the European Stroke Organization (ESO), the European Society of Minimal Invasive Neurotechnology (ESMINT) and the European Academy of Neurology (EAN) and a large patient organization (SAFE), and we are conducting a survey throughout Europe in order to create a map to show the areas where these procedures are performed and where there is still a lack of these interventions.
A map like this will allow us to target healthcare politicians and those within the government to convince them as to why investment in this therapy is so important. As there are many benefits, such as reducing handicap, saving lives, and preventing recurrent stroke. In addition to this, there are studies showing that these interventions are highly cost effective.
What exciting innovations are currently in the pipeline?
There is still a lot more to come, although now we know that stent retrievers are working, there are still a lot of unanswered questions.
We have four arteries leading to the brain, anterior and posterior, and currently stent retrievers are only approved for patients with large occlusions in the anterior circulation.
This is because they have been proven to be effective in the anterior circulation but for the moment there is no evidence in the posterior circulation. Based on our experience, I am fairly confident they will show similar efficacy in the posterior circulation as the anterior, but studies have to be performed.
Furthermore, there are other unanswered questions such as: Which patient should be treated with intravenous thrombolysis, which patient should be treated with the catheter? What is the upper time window for endovascular interventions? Does this time window vary between specific patients? This last question is particularly important because some patients come in late and we don't know whether we can treat them or not.
In terms of innovation, there are a lot of new techniques in development. There are new recanalisation devices in the pipeline, which aim to recanalize smaller vessels and which aim to test new treatment approaches such as aspiration.
Some of these techniques are currently assessed in randomized trials. Imaging is also very important because CT and MRI are important to selecting the right patients for the right treatments and therefore we need more studies to help us to select the right patient for the right treatment.
My dream for the future would be a one-stop procedure that the patient coming in with an acute stroke could be investigated and treated in one single room. Patients would be examined there, then they can be scanned immediately and then the intervention could be started in the same room.
This would mean you don't have to move the patient first to the CT then to the Angio suite and so on. This method would be the most beneficial for the patient by reducing time delays and I think in the near future it is feasible to have this.
At what stage of development are these innovations currently at?
Currently it is possible to combine a CT scanner and an Angio suite within one room, but adding the MRI and angiography within one room is still more difficult. I think in some years it might be possible to have such a stroke room, that I mentioned in the previous question.
Similarly, in cardiology, they are no longer taking patients with chest pain to the emergency room, instead they're being taken directly to the coronary lab for the reopening of the coronary arteries.
It is more complicated in stroke because it is not always known whether the patient has a stroke, an intracerebral haemorrhage or another neurological disease. Therefore, you need imaging first before you can start treating the patient. But I think in the near future it will be possible to have everything in one single room.
How important is innovation in stroke treatment?
Innovation is very important, as we have a lot of unanswered questions, we need even better devices than we have now, we need complete recanalization within even faster time periods because in stroke treatment time is brain. You have to treat the patients as fast as possible and therefore this needs to be quicker.
We need to be able to bring the right patients to the right center as fast as possible. Pre-hospital patient selection is therefore very important, because ideally patients with suspicion of an acute stroke with a large vessel occlusion should be directly referred to a center, where these endovascular procedures can be performed whereas patients with a small vessel occlusion should be sent to the nearest stroke unit, where intravenous thrombolysis can be started without time delay.
However, clinical identification of patients with large and small vessel occlusions is still a major challenge. In Switzerland, where I am working, there are nine certified stroke centers, which can perform endovascular procedures and fourteen stroke units, where intravenous thrombolysis can be performed.
This model guarantees a coverage of the Swiss population (8 million people). Current estimations suggest that you need roughly one stroke center per one million people, but different areas vary in density. For example, in Norway, you cannot have the same density of stroke centers as you probably have in central London.
We need also innovation in terms of how we can get patients to the right center as fast as possible. There are several possibilities. Stroke ambulances are ambulances that have a CT scanner integrated in the vehicle. Imaging can already be performed in front of the patient’s house and intravenous thrombolysis can be started. If the patient has a major vessel occlusion they can be transferred to the next stroke center.
This is an innovation which is most useful for urban areas, such as London and Berlin. It's less useful in remote areas like Norway, as an ambulance can take many hours to get to the patient. There it would be much easier just to bring them to the next hospital, either by ambulance or helicopter. But these are different aspects which need to be answered and solutions must be tailored to the different geographical regions throughout Europe.
What are the main barriers you see?
One of the most important barriers is the cost. Building up stroke centers is quite expensive for a hospital and for a healthcare system. Angio suites are required, around the clock supervision is needed and this is a major problem, costing a large investment from the hospital.
Furthermore, we don't have a national or even European strategy of stroke management. In Switzerland, the government decided that stroke treatment is highly specialized medicine and only certified professionals should perform this procedure. There are nine stroke centers and 14 stroke units currently in Switzerland, which are well-balanced throughout the country. I think this is a prime example of how stroke treatment should be organized in an area.
How does innovation for stroke treatment vary by country across Europe?
As mentioned previously, countries like France, Germany, Switzerland and Catalonia have high standards regarding endovascular stroke therapy and there are sufficient stroke centers that can perform these endovascular procedures.
However, there are other areas throughout Europe where these interventions are not performed or only in major urban areas. Currently there is no data for the number of centers throughout Europe, and that's the reason why we want to perform the survey I mentioned earlier.
How can we improve stroke prevention?
Acute stroke treatment is very important, since we can reduce the handicap in stroke survivors. But it is equally – or even more - important to prevent strokes, since preventing strokes is much more effective than trying to reduce the handicap once a stroke has occurred..
Public campaigns informing people on stroke risk factors is of major importance. For example, hypertension is the most relevant risk factors for stroke and if treated effectively many strokes could be prevented. Other risk factors include: high cholesterol, diabetes, smoking, obesity, lack of physical activity, etc. The public needs to be encourage to take responsibility for their health.
Raising awareness of the signs and symptoms of a transient ischaemic attack (TIA) and stroke is also very important. Patients have to be able to recognise these symptoms and they have to know, that occurrence of these symptoms is a medical emergency and immediate consultation in an emergency room is mandatory
There is often a situation where a patient who has suffered a TIA and had neurological symptoms for a brief period of time, does not visit a physician once the episode has passed. This is a major problem because the risk of having a subsequent major stroke within the next few hours and days is extremely high after a TIA and should therefore be treated as an emergency.
A stroke and a TIA is in most cases not painful, like a myocardial infarction is, and so patients often do not seek medical attention following an attack.
What support is there for patients following a stroke?
There is a lot of attention surrounding acute stroke treatment, however it is also important to think about the care for those who have suffered a stroke, which gets a lot less attention.
Patient recovery is very important and should not be forgotten, as well as the support for the families and the relatives of those who suffered a stroke. There needs to be more organizations that focus on taking care of patients and relatives following a stroke.
Where can readers find more information?
For the general public:
More suitable for professionals:
- The European Stroke Organization: https://eso-stroke.org/ - this website is more suitable for professionals. About Professor Urs Fischer
About Professor Urs Fischer
 Urs Fischer is Professor for Acute Neurology and Stroke at the Department of Neurology and Co-Director of the Clinical Trial Unit (CTU), University of Bern.
Urs Fischer is Professor for Acute Neurology and Stroke at the Department of Neurology and Co-Director of the Clinical Trial Unit (CTU), University of Bern.
He studied in Bern, London, San Francisco and Lomé and graduated in 2000. He trained as a neurologist in Bern.
In 2008/2009 he performed a master of science by research in Clinical Neurology at the University of Oxford. In 2014 he became an associate professor and in 2015 he was elected as Professor for Acute Neurology and Stroke at the University of Bern.
He is the Co-Chair of the Stroke Center Bern and Head of the Neurological Emergency Team. Furthermore he is the Co-Director of the Clinical Trial Unit at the University of Bern.
Urs Fischer is a clinical researcher and his main research interest involves diagnosis, management, treatment and outcome of patients with acute neurological diseases, especially of patients with acute ischemic and hemorrhagic stroke.
He is participating in multiple preventive, diagnostic and acute treatment trials and stroke registries. He is Co-PI of the SWITCH study and PI of the ELAN safety study.
Urs Fischer is active in National and European Stroke Societies: he is Secretary General of the European Stroke Organisation (ESO) and together with Prof. Jan Gralla he founded the ESO ESMINT ESNR stroke winter school, will be held for the fourth time in Bern in February 2017.