Feb 21 2017
Researchers at Okayama University report in the December 2016 issue of the American Journal of Cancer Research a novel in vivo model for the study of pancreatic ductal adenocarcinoma (PDAC) tumors. The model relies on induced pluripotent stem cell conversion; the artificially generated cell lines exhibit the PDAC phenotype and are expected to help our understanding of pancreatic cancer.
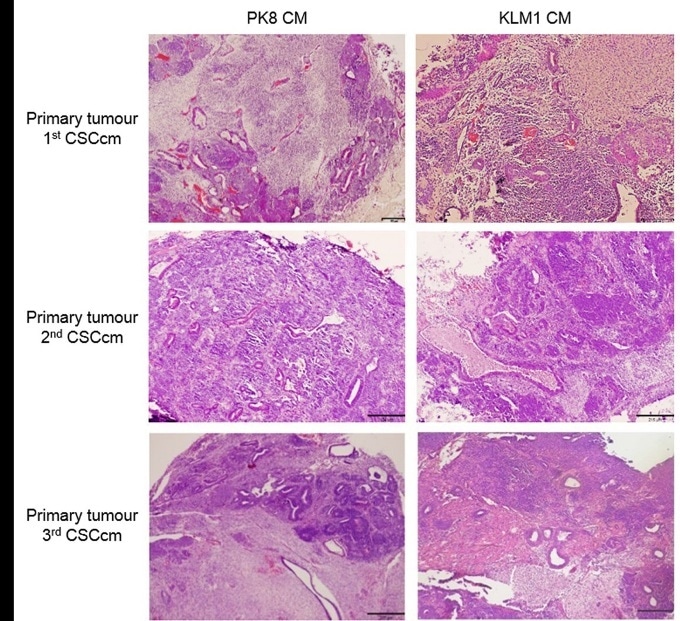
Sections from serial primary tumors showing the histopathological adenocarcinoma-like morphology. H&E staining. Original magnification 4×. Tumors from subcutaneous transplant (1st CSCcm) displayed adenocarcinoma-like histopathological morphologies whereas orthotopic primary tumors (2nd and 3rd CSCcm) showed PDAC-like structures, richer in stroma mostly located in the inner mass. PK8 CM and KLM1 CM are the miPSCs treated with the conditioned medium from human pancreatic cancer cell lines PK8 and KLM1 respectively.
Pancreatic ductal adenocarcinoma (PDAC) tumors, typical manifestations of pancreatic cancer, are known to be strongly resistant to radiation therapy and chemotherapy. For finding a cure for the disease, it is essential to develop representative mouse models of PDAC tumors. An international team of researchers including Masaharu Seno and colleagues from Okayama University have now devised a new method for generating PDAC tumors in vivo — providing a promising platform for investigating pancreatic cancer.
Among the different types of cells that are present in a PDAC tumor, cancer stem cells are the ones associated with tumor initiation. Using the technique of induced pluripotent stem cell (iPSC) conversion, the researchers generated in vitro pancreatic cancer stem cell lines (CSCcm) in the lab that have properties of cancer stem cells. The iPSC-converted cell lines led, after being transplanted into mice, to tumors with the PDAC phenotype, which can hence serve as models for the study of PDAC occurrence and progression.
The researchers point out that, importantly, their approach involves no genetic manipulation. Indeed, until now, mouse models used for studying pancreatic cancer were usually genetically engineered — a problem when trying to understand spontaneous tumor occurrence.
In order for the in vitro iPSC-converted cell lines to develop the features of cancer stem cells, they need to be introduced into a mouse or other organism, which is not ideal. “This reliance on in vivo systems is an unresolved matter that must eventually be overcome,” says Seno.
The researchers already used their novel model to address the issue regarding certain single-point mutations often seen in PDAC tumors. A preliminary analysis shows that these mutations are not observed for the CSCcm lines, and that there is therefore no correlation with tumor initiation. Future research based on this mouse model is expected to lead to further valuable insights into the origin of pancreatic cancer that might ultimately lead to a cure.
Background
Induced pluripotent stem cells (iPSCs) and regenerative medicine
Stem cells are cells that have the ability to differentiate — that is, become cells of a specialized type. An important attribute of a stem cell is its potency, indicating into what types of cells the stem cell can differentiate. So-called pluripotent stem cells (PSCs) can develop into organisms, because they can differentiate into cells of any of the three different germ layers characteristic of organisms.
An induced pluripotent stem cell (iPSC) is a PSC artificially generated from a non-PSC. The procedure for creating iPSCs was discovered in 2006 by Shinya Yamanaka. Nowadays, iPSC generation is a promising technique in the field of regenerative medicine: damaged or badly functioning human cells can be replaced by cells properly differentiated from iPSCs.
Seno and colleagues used a technique based on iPSC conversionwhere they converted iPSC lines into cancer stem cells that mimic pancreatic cancer stem cells.
Pancreatic ductal adenocarcinoma (PDAC) tumors
The most common form of pancreatic cancer is pancreatic ductal adenocarcinoma (PDAC). PDAC tumors consist of different types of cells: cancer stem cells (CSCs), differentiated cancer cells, tumor-associated pluripotent cells and immune cells. For induced pluripotent stem cells (iPSCs) to be converted into cell lines leading to valid mouse tumor models, they have to be sufficiently similar to the CSCs, as these are the ones believed to be linked to tumor initiation. The researchers were able to confirm that their iPSC-converted cell lines recapitulated the PDAC tumor phenotype — which signifies an important step towards new diagnostic approaches and a better understanding of PDAC tumor origin and progression.