Researchers at The University of Manchester have discovered that a protein (5T4) found on the surface of cells contributes to chemotherapy resistance in the most common type of childhood leukaemia. Using a novel approach, early testing shows that targeting the protein with an antibody drug conjugate (ADC) could hold promise in improving treatment.
The research, which was funded by the blood cancer charity, Bloodwise, is published in Haematologica.
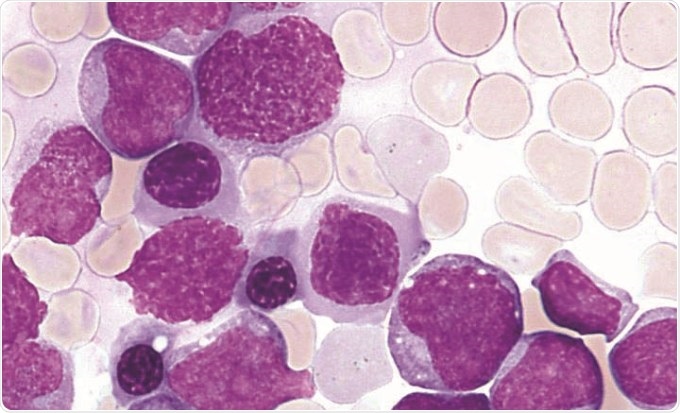
Survival rates for childhood acute lymphoblastic leukaemia (ALL) have improved substantially over the years. Now, around nine in 10 children can look forward to being cured, but current treatment – usually an intense course of chemotherapy – is gruelling and can leave children with life-long side effects such as infertility and even secondary cancers. There is also a chance of the blood cancer returning if high levels of leukaemia initiating cells remain after the first rounds of intensive treatment. If the cancer comes back, it is more difficult to treat.
In a study led by Professors Vaskar Saha and Peter Stern, researchers analysed samples from children who were determined to be at either low or high risk of relapse based on the numbers of leukaemic cells remaining after their first round of chemotherapy.
The researchers found a high proportion of 5T4 positive leukaemia cells in patients with a high risk of relapse, while this marker was not detected in samples taken from children who responded well to initial treatment.
5T4 positive leukaemia cells are significantly more clonogenic. This means that the disease can recur from very few residual cells. The researchers discovered that the 5T4 protein helps leukaemia stem cells migrate from the blood vessels to the safety of the bone marrow during treatment, which offers protection from chemotherapy and makes these cells much harder to eradicate.
Using a model system of human leukaemia engrafted in mice, an ADC developed by Pfizer Inc., A1mcMMAF, which targets cells with 5T4 molecules on the surface and delivers a drug which is toxic for the cells, was shown to be very effective in treatment. In addition, when used in combination with dexamethasone, a standard component of induction therapy, there was a significantly improved survival of the mice.
Professor Vaskar Saha, who led the research with Professor Peter Stern at The University of Manchester, said:
Although this is early work, our findings suggest that leukaemic initiating cells that have 5T4 are better at entering sites in the body that will protect them from standard chemotherapy, causing drug resistance and relapse. By targeting 5T4 in mice, we have shown that we can selectively attack the treatment-resistant leukaemia cells.
Dr Alasdair Rankin, Director of Research at Bloodwise, said:
The chemotherapy currently used to treat childhood ALL is not always effective, and can cause life-long side effects. Using targeted therapies – alone or in combination - that hone in on specific characteristics of the cancer cells, could eventually make therapies gentler and more effective. These early findings are promising, and have opened up the future possibility of a new targeted treatment for childhood ALL.