An interview with Gilberto Dalmaso, discussing the different grades of pharmaceutical cleanrooms and the production of high-level compounds under aseptic conditions.
Please give an overview of different processes used when considering microorganisms in pharmaceutical production.
In the pharmaceutical industry, there are two main processes - non-sterile and sterile production. Non-sterile production includes tablets, syrups, ointments, and capsules. From a regulatory point of view, the processes can be microbiologically contaminated but within specified microbiological limits.
Then we have sterile products which, are mainly products that are injected or in direct contact with open wounds. They must be completely free of microbiological contamination and manufactured in a clean, controlled environment.
 warut pothikit | Shutterstock
warut pothikit | Shutterstock
Within the sterile category there are two types of products: those that are terminally sterilized, i.e. produced and then sterilized at the end of production in big autoclaves to kill all the microorganisms, or those that are produced aseptically, with no terminal sterilization. Aseptically means that all the steps of the process should be sterile, without microbiological contamination.
Why are there different processes that require different levels of sterilization? Why are tablets and some other pharmaceuticals allowed to not be aseptically produced?
When you produce tablets, capsules, ointments, syrups, and creams, microbial contamination is allowed, to a certain extent because you put these items on the skin or ingest them through the mouth, so the administration is not a sterile route, but rather one that is constantly exposed to contamination.
When you use an injectable, the route of administration is sterile: directly into the body or blood. Any non-sterile components introduced into the production process is done in clean rooms to manage possible contaminants. Contamination should be zero if possible, and should be controlled within established parameters.

What considerations are taken into account when producing compounds that need to be aseptically prepared?
Aseptic processes are performed in a clean and controlled environment, free of microbial contamination. Otherwise, your product will also become contaminated. In my opinion, this kind of production should be as controlled as possible, not just the minimum amount needed to meet regulatory requirements.
The microbiological aspects, microbiological issues and microbiological controls should be very important to avoid any possible dangerous contamination.
Aseptic production processes start from the compounding of all the raw materials, where they are mixed together. In many cases, they are dissolved in water before being filtered with sterilizing filters to enter into the filling machine.
The same process considerations need to be taken with the filling machine, which has to be completely sterile. The final containers include vials, ampules, syringes, and bags which must be pre-sterilized.
Once filled, the containers have to be closed and sealed to maintain the sterile environment with sterile stoppers, aluminium seals or, for ampules, by flames, before packaging.
What measures are generally put in place to provide quality assurance for aseptic processes?
Regulatory authorities all over the world, including the EMA in Europe and the FDA in the US, issue procedure guidelines which represent the minimum requirements that pharmaceutical companies should deploy to ensure aseptic processes.
These procedures are primarily required in clean rooms, where production takes place and potential contamination is controlled. There are many guidelines from how the air flows and is filtered to how possible contamination and room conditions are monitored, and then how data is stored and reported.
The air must be filtered by HEPA filters to retain particles and microorganisms.
People enter controlled areas wearing sterile cleanroom garments, and the controlled areas are monitored in terms of temperature, humidity and total particles. There are also microbiological controls to avoid introducing microbiological contamination.
In clean rooms there are filling machines, which are protected from the operators during production because operators are the main source of microbiological contaminants in the environment. Our bodies are full of, and covered by microorganisms, so we can easily introduce contamination without the right barriers.
The filling machine areas, including air, surfaces and operators, are monitored by particle counters and microbiological monitors. The compressed gasses that are used in the filling machine are also monitored. All the materials that are used are sterilized by autoclaves or ovens.
These are the main, required monitoring procedures of the ‘GMP’ (Good Manufacturing Practices) issued by the authorities.
How do aseptic processing quality assurance measurements change across, solid, liquid and gaseous testing samples?
There are various methods, which largely change based on the sample media, whether you are measuring viables or non-viables, and how samples are collected to perform tests.
For particles in liquids, samples are taken from the solutions within the process using something like an APSS 2000 particle counter. For viables in liquids, samples are taken from the solutions within the process, to do a laboratory sterility test.
The product is put in a culture media. If there are microorganisms present they will grow in the media; the turbidity of the culture media and that it's contaminated will be seen.
For surface quality assurance swabs are used to check for microbial contamination. A swab sample is taken from the surface and put into the growth media to check for microorganisms. A rapid method example of this procedure is using a SurCapt Kit.
For cleanroom air, you sample the air as it continues its unidirectional flow. For microbial testing the air is impacted on to the culture media (for example, using a BioCapt).
Microorganisms in the air interact with the culture media and grow so the contamination can be seen. For particles, the air is collected and counted using a particle sensor such as an Airnet or a counter like a Lasair III.
How does the total level of particulates affect the likelihood of airborne microorganisms in a cleanroom? Does having lower particulate levels necessarily make for a more sterile environment?
GMPs for aseptic processes require that there are no more than 3,520 particles greater than 0.5 microns per cubic meter (learn more by reading ISO 14644-1:2015 Revisions Summary.) Particle counters provide real-time data and let cleanroom operators know right away if there is a change in the cleanroom condition.
If there is a change, cleanroom managers can quickly investigate the problem. However, particle counters don’t reveal how many of the particles within the cleanroom are viable. So, if the process has only 2000 particles greater than 0.5 microns, the process adheres to industry standards.
However, we don't know, within these 2000 particles, how many viable and potentially harmful particles we have. Only a microbial monitor can tell us if the particles are viable.
These two different types of contamination monitoring methods use different approaches: microbiological methods grow microorganisms in media, while particle counters use physical counting methods and an optical chamber to tally the particles in the air.
However, a particle counter doesn't know whether the particles are viable or non-viable. Ultimately, pharmaceutical cleanroom operators need to know when there is viable contamination in the cleanroom.
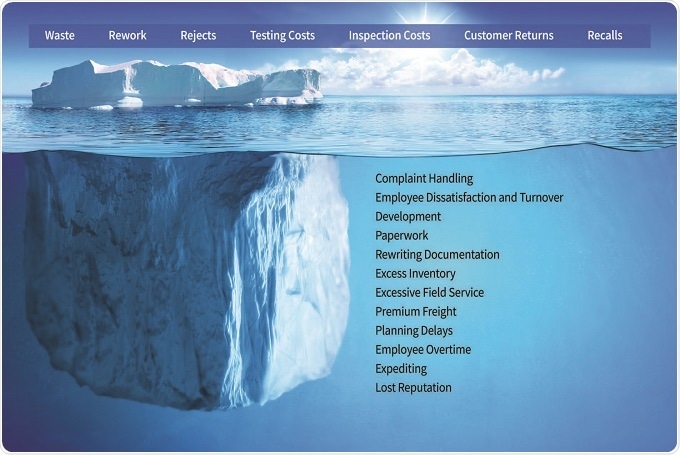
What are the consequences of poor aseptic control in cleanrooms?
The consequences are enormous: that potentially harmful viable microorganisms enter in our aseptic sterile products and cause critical health problems. To see microbiological contaminants and to know whether processes and products are at risk of contamination, it is essential to employ the best technologies and approaches.
New technologies in microbiology are much more sensitive, faster, and give you more information of the process.
What solutions do Particle Measuring Systems provide for the measurement of aseptic processes?
Particle Measuring Systems is investing and growing in several ways to support pharmaceutical cleanroom monitoring. We can now provide our customers with the right products (microbial and particle as well as FMS systems), GMP services, and have a team of subject matter experts who can be brought it to advise our customers on their processes and help them to improve their contamination control in all areas and at all stages.

Our Advisory Team has vast experience in the processes and can support the customer to implement their contamination control based on quality by design, rather than trying to control it at the end of the design process.
Particle Measuring Systems continues to support our customers with contamination monitors for microbial and particulates. We are continually investing in new products and improving the scope and capabilities of our existing products that have been setting the industry standard for years.
We strongly believe that new technology should, especially in microbiology, be implemented in projects as soon as possible, to make sure cleanrooms are maintaining the highest assurance of sterility.
Our newest microbial products include the BioCapt Single-Use Microbial Impactor for continuous monitoring of viables in the air. We have the Minicapt for mobile or remote microbial monitoring. We also have the SurCapt Kit for surface contamination monitoring.
We also provide environmental monitoring solutions and software to help our customers get instant access to all facility data immediately and set and respond to contamination alarms, while also ensuring data integrity and reporting that meet regulatory requirements.
What does the future hold for aseptic processing quality control? What cutting edge techniques or technologies are there in this field?
My dream is to have a process where there are no people involved because they are usually the main source of product contamination. I’d like to see a completely automated manufacturing process where all steps of the process are completely evaluated in terms of sterility assurance.
The future of aseptic processes are technologies that monitor microbiological contamination of the process in real time and speciate, combined with automatic sterilization of the line, which would increase sterility assurance dramatically.
Where can readers find more information?
Particle Measuring Systems has an online Knowledge Center, available for free to the public. There they can find papers and webinars such as Ensuring a Successful Audit or Identifying the best rapid microbial monitoring solution for your critical & ISO 5/ Grade A surfaces
About Gilberto Dalmaso, Ph.D
Senior Consultant and Pharma Customer Advisory Team Manager: Life Sciences Division: Particle Measuring Systems
 Gilberto Dalmaso has over 25 years’ experience in pharmaceutical microbiology and sterility assurance, primarily with GlaxoSmithKline (GSK). Over his last five years with GSK, Gilberto led a series of initiatives implementing Process Analytical Technologies (PAT) and Rapid Microbial Methods (RMM) that improve quality and process understanding while yielding significant cost savings.
Gilberto Dalmaso has over 25 years’ experience in pharmaceutical microbiology and sterility assurance, primarily with GlaxoSmithKline (GSK). Over his last five years with GSK, Gilberto led a series of initiatives implementing Process Analytical Technologies (PAT) and Rapid Microbial Methods (RMM) that improve quality and process understanding while yielding significant cost savings.
In 2003, his laboratory gained the distinction of obtaining the world’s first rapid microbial PAT approval from the US FDA. Today Gilberto is the Global Aseptic Processes Development Manager for Particle Measuring Systems.
In this role, he collaborates and consults with pharmaceutical companies to develop and implement science-based strategies and processes that utilize Quality by Design (QbD) principles to monitor, control, and improve the chemical, physical, and microbiological state of various production processes.
With his extensive experience in sterility assurance and microbiology, Gilberto has the capability of supporting pharmaceutical manufacturers in a wide variety of aseptic processes, machinery, technologies and methods.