Researchers have developed a novel technique where molecules would be motorized using light and these would be used to drill holes in the membranes of individual cells such as the cancer cells. This could bring the treatment molecule into the cancer cell directly and cause them to die.
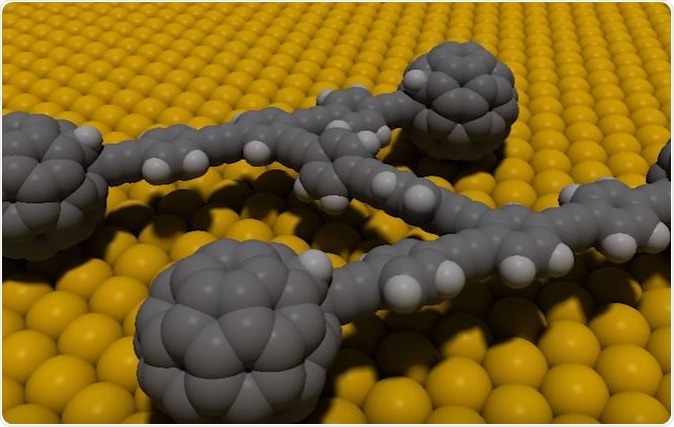
Rice University nanomachines constructed to deliver drugs, destroy diseased cells. Image Credit: Rice University
This technique would save the millions of normal healthy cells that are killed by the traditional chemotherapy agents when they attempt to kill the cancer cells. The study was published in the journal Nature.
The study led by Dr Robert Pal Department of Chemistry and Biophysical Sciences Institute at Durham University was worked upon by researchers Professor James Tour from Rice University, Houston, and Assistant Professor Gufeng Wang from North Carolina State university. Rice graduate student Victor Garcia-López is lead author of the study. Co-authors of the study include graduate students Lizanne Nilewski and Amir Aliyan, research scientist Guillaume Duret, Anatoly Kolomeisky, a professor of chemistry and chemical and biomolecular engineering and Jacob Robinson, an assistant professor of electrical and computer engineering from Rice and Fang Chen from North Carolina State.
The team worked to develop rotors in a single-molecule nanomachine which could be activated by using ultraviolet light to spin at two to three million rotations per second. This would act a s a drill that would open membranes in cells.
As an initial step the researchers tested these microscopic motorized cells to target cells from prostate cancer. Within activation, these molecules took from one to three minutes to kill the cancer cells said Dr. Pal. The attacked cells showed bubbles on their surface called blebbing followed by their death.
Rice University nanomachines constructed to deliver drugs, destroy diseased cells
Dr Pal believes that this technique could mean that a wide variety of cancers could be treated using these tiny machines. Dr Pal, a Royal Society Research Fellow, added that these “light-activated nanomachines” would be able to target cancer cells including those that are difficult to treat or resistant to treatment. This is a step towards change in the “non-invasive” cancer treatment he said. This means, cancer treatment no longer has to be debilitating for the patient. Further this treatment would improve survival rates greatly worldwide and thus benefit millions of patients. Dr James Tour added that these nanomachines are so small that around 50,000 of them could be placed across the diameter of a single human hair. But these can be used to target specific cells with great accuracy.
Nobel laureate Bernard Feringa won the Nobel prize for chemistry in 2016 for developing these microscopic motors. The motors are a paddle-like chain of atoms which can move in one direction when they are provided with energy.
The Rice laboratory created the motor-bearing molecules in more than one size. In addition they also made peptide-carrying nanomachines that could home in on the target cells and kill them. North Carolina State University worked to test these nanomachines on synthetic replicas of the cell membranes which these molecules successfully broke apart.
The next step was tested at the Durham University where these motorized molecules were tested on live cells including human prostate cancer cells. This last step showed that the mototrized molecules reached the target cells and stayed on the surface. They would drill into the cancer cells only when activated using UV rays.
The researchers are working on other methods that could activate these motors such as two-photon absorption technique, near-infrared light or radio frequencies. This would allow for an easier and more cost effective photodynamic therapy.
The research received support from the National Science Foundation, North Carolina State University, the Royal Society and the Biophysical Sciences Institute at Durham University. At present the team is progressing to work on microbes and small fish. Soon they would work on laboratory rats and mice. Once animal testing is successful, clinical trials could begin for humans.
References