Kate Bass BSc
Novel bifunctional immunotherapeutic agents have been developed that, in addition to inactivating key immune checkpoints, also deactivate the tumor's protective response.
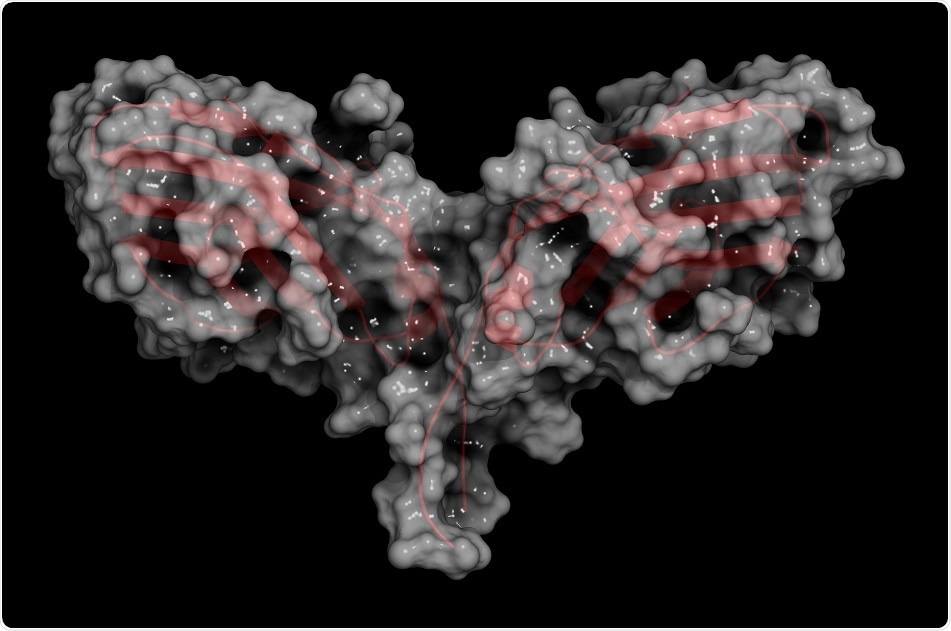 Credit: molekuul_be/ Shutterstock.com
Credit: molekuul_be/ Shutterstock.com
Cancer immunotherapy has been heralded as the most promising new cancer treatment strategy since the development of the first chemotherapies seven decades ago. It uses the innate powers of the immune system to fight cancer.
The high specificity of the immune system means that it can be used to direct treatments to a selected tumor target. In this way the toxic compounds needed to eliminate cancer cells are delivered to the target area, minimising the impact on healthy tissue.
Immunotherapy has proved to be particularly beneficial in patients with certain types of cancer that have been resistant to chemotherapy and radiation treatment. However, it is also an approved first-line treatment for several cancers.
Cancer cells protect themselves from the host's immune system by activating natural mechanisms that suppress the immune system. This includes increased production of the immune suppressors CTLA-4 and PD-1/PD-L1. Immunotherapy involves administering antibodies specific to these proteins, which locate, bind and deactivate them.
Despite the great success achieved with immunotherapy, the responses are not maintained in many patients. Such failure has been attributed to the ability of tumors to produce transforming growth factor-β (TGFβ) that regulates the expression of immunosuppressive regulatory T cells (Tregs).
Using information on the TGFβ activation pathway gleaned using artificial intelligence, researchers have developed a new class of bifunctional immunotherapeutic agents. In addition to inhibiting immune suppressors, such as CTLA-4 and PD-1/PD-L1, these agents also deactivate TGFβ.
The novel immunotherapy agents comprise an antibody for either CTLA-4 or PD-L1 fused to a TGFβ trap that mimics the natural TGFβ receptor.
This new type of immunotherapy has achieved significant inhibition of tumor growth, even when used against cancers that did not respond to available immunotherapies, including the anti- CTLA-4 treatments ipilimumab and pembrolizumab, and the anti-PD-L1 agents atezolizumab and avelumab.
Since these mechanisms of immune dysfunction are shared across many types of cancer, the Y-trap approach could have broad impact for improving cancer immunotherapy"
Atul Bedi,M.D., Johns Hopkins University School of Medicine
Robert Ferris, professor of oncology at the University of Pittsburgh, agreed that "This approach appears to be an innovative strategy, and an exciting technical accomplishment to target multiple suppressive mechanisms in the tumor microenvironment".