Fecal microbiota transplantation or stool transplant from a donor is useful for patients infected with the deadly recurrent Clostridium difficile that leads to severe diarrhea, pain and often serious consequences.
Fecal transplant is also useful in patients who suffer from inflammatory bowel disease or ulcerative colitis. It has been seen that some people prove to be better stool donors compared to others. A team published their findings on this in the latest issue of the journal Frontiers in Cellular and Infection Microbiology.
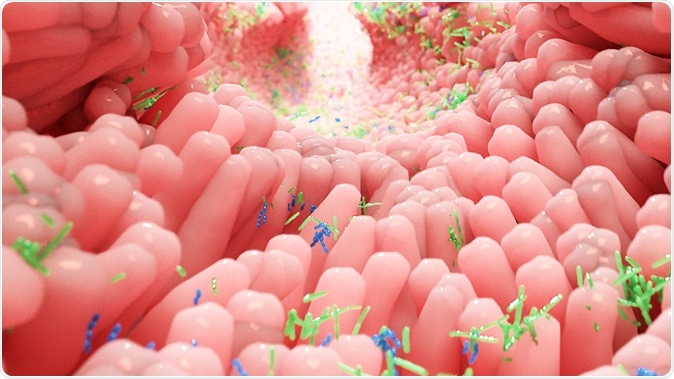
Human microbiota in intestine - Illustration. Image Credit: Alpha Tauri 3D Graphics / Shutterstock
Donors whose fecal transplants produce better results are called “super donors”. A team from the University of Auckland looked at faeces samples and microbes within them from the donors. These samples are often transplanted to the gut of patients with C. difficile infection to “re-set” the gut and make it function again. The donor dependent results are not commonly seen among patients who suffer from C. difficile infection but results are marked when the transplants are used in patients of ulcerative colitis. Researchers explain that the gut microbiome of the donors could play a role in their being better donors.
Dr Justin O’Sullivan and colleagues write in their study that recurrent C Diff infections occur due to the over population of certain bacteria. In ulcerative colitis there is a complex within the gut and here this “super donor effect” is visible. O’Sullivan explained that there are several factors that affect the recovery of the recipient and a deeper look into this super-donor effect can help treat the condition better.
O’Sullivan and colleagues write that samples from the super donors seem to have a rich diversity of microbes in them. “We think the super-donors differ depending on the condition you are trying to treat,” said O’Sullivan. They also speculate that there may be compatibility issues between the donor and the recipient and the species and strains of microbes from the donor and the recipient may be interacting with each other. They also add that diet of the donor and recipient is a major factor that determines the success of the process.
The researchers conclude in their work that the approach of “one stool fits all” is mistaken and each donor needs be personalized for the recipients. They also speculate that other patients such as those of atopy and asthma may also benefit from the procedure if the actual principle behind the success of certain donors is found.