Feb 14 2019
Previous FDA Approval Could Fast-Track Much Needed Treatment
An antidepressant drug used to treat obsessive-compulsive disorder could save people from deadly sepsis, new research from the University of Virginia School of Medicine suggests.
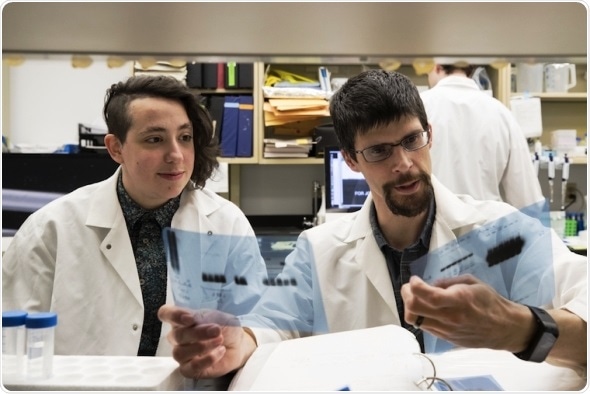
Researchers Dorian Rosen (left) and Alban Gaultier, PhD, have identified an antidepressant that may also stop deadly sepsis.
Sepsis is a significant cause of death around the world. The federal Centers for Disease Control and Infection calls it “the body’s extreme response to an infection.” Essentially, the body’s immune response spirals out of control, and the normally beneficial inflammation becomes harmful. The result can be tissue damage, organ failure or even death.
Sepsis is very dangerous. In the U.S., 1.7 million get it every year, and 270,000 people die. Once you get diagnosed, you have a high chance of mortality. And there is no good treatment. Basically, we will try to keep you alive and monitor you as much as we can. So clearly there is a critical need for treatment.”
Alban Gaultier, PhD, researcher, UVA’s Department of Neuroscience and its Center for Brain
Gaultier and his team have identified a drug that could offer that treatment – and previous safety testing of the drug could fast-track it into use in hospitals around the country.
A Simple Solution for Sepsis?
The UVA researchers were looking at a little-studied biological process inside our cells when they determined it has an important role in regulating inflammation. He began studying it partly because there are already drugs that can affect players in the process.
“Inflammation, most of the time, is good. It’s when it gets out of control that we need to modulate it,” Gaultier said. “Inflammation is a very precisely controlled reaction. When we need it and have too much, it’s a problem, but when we don’t have enough, it’s also a problem.”
To evaluate the potential of one drug, the antidepressant fluvoxamine, to stop sepsis, Gaultier’s team tested it in a mouse model of the disease. Only 9 percent of the mice given fluvoxamine died, compared with 62 percent of the untreated mice.
While the drug will need to be tested in people to determine its effectiveness at battling human sepsis, previous testing to determine its safety should accelerate that process.
Gaultier hypothesizes that the same biological process could be targeted to generate beneficial inflammation when needed, such as in immunocompromised people. “By inhibiting the receptor, we could activate inflammation in conditions where patient don’t have a proper inflammatory response,” he said.
He plans to continue his research, including testing that hypothesis.