A new software tool has proved to be four times more reliable than current methods at predicting prognosis in patients with ovarian cancer. The tool was also able to predict the most effective course of treatment for patients once they had been diagnosed.
 Fancy Studio | Shutterstock
Fancy Studio | Shutterstock
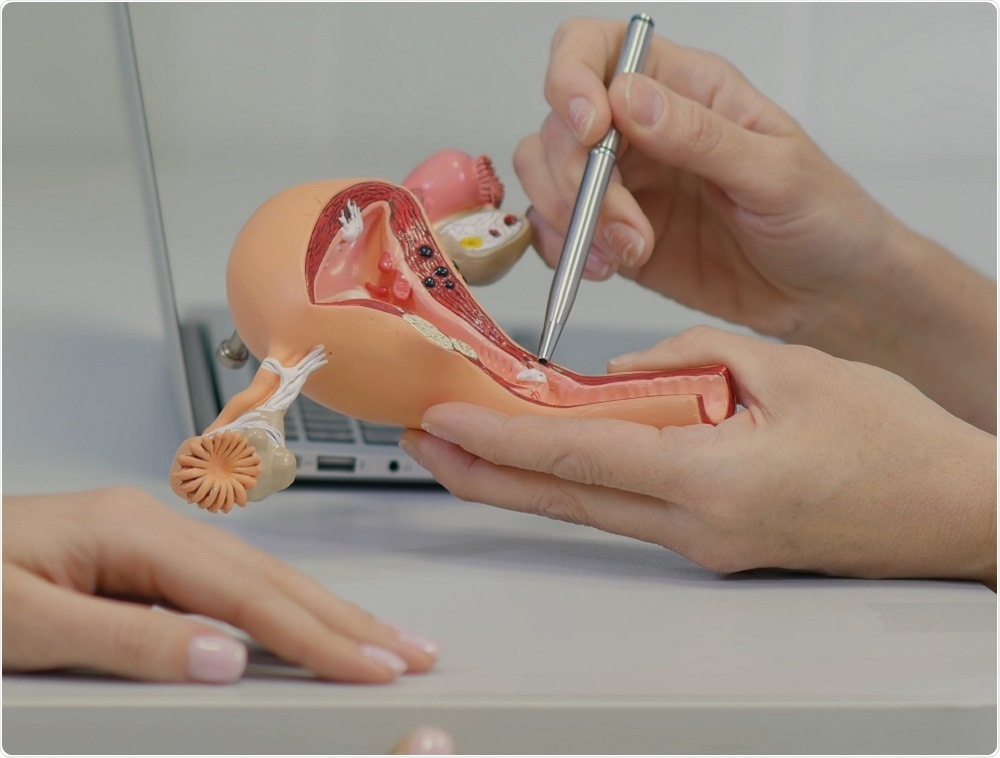
Ovarian cancer is the sixth common cancer in women and mostly affects those who have gone through the menopause or those with a family history of the disease.
The long-term survival rate is only 35 to 40%, since the cancer is often only diagnosed during the later stages, once symptoms have already started to present. The ability to detect ovarian cancer at an earlier disease stage is urgently needed and could improve patient survival rates.
Currently, diagnosis of ovarian cancer involves a blood test for a substance called CA125 (a cancer indicator) and a CT scan that generates detailed images of ovarian tumors. These tests can help doctors see how far the cancer has spread and whether a patient may benefit from surgery or chemotherapy, for example. However, these tests do not reliably indicate how effective that therapy may be or the likelihood of survival.
As reported in the journal Nature Communications, researchers at Imperial College London and the University of Melbourne have now used a piece of mathematical software to assess tumor aggressiveness using CT scans and tissue samples taken from 364 patients with ovarian cancer between 2004 and 2015.
The software assessed four tumor characteristics (structure, size, shape and genetic make-up) that are known to influence patient survival. This generated a score called the Radiomic Prognostic Vector (RPV) that serves as an indicator of disease severity.
On comparing the RPV score with the blood tests results and prognostic scores doctors currently use, the team found it was up to four times more reliable at predicting patient death. It was also able to reliably identify the 5% of patients that would usually only survive for two years.
Identifying those patients early on enabled the team to better determine the most effective therapy and improve prognosis.
Researchers say the technology could help clinicians optimize treatment earlier on and lead to a more personalized approach to therapy:
Artificial intelligence has the potential to transform the way healthcare is delivered and improve patient outcomes. Our software is an example of this and we hope that it can be used as a tool to help clinicians with how to best manage and treat patients with ovarian cancer.”
Professor Andrea Rockall, Co-Author