Research published yesterday in The New England Journal of Medicine describes how an antibody that prevents HIV binding to human immune cells was shown to be able to suppress levels of HIV for up to four months.
 Kateryna Kon | Shutterstock
Kateryna Kon | Shutterstock
Human Immunodeficiency virus (HIV) severely damages the immune system, eventually leading to Acquired Immunodeficiency Syndrome (AIDS) which is fatal and has no cure. At present, the World Health Organization (WHO) estimates that around 34 million people in the world are living with HIV.
Patients infected with HIV are currently treated with a cocktail of antiretroviral drugs designed to prevent the replication of the virus within the body and delay the onset of AIDS. Although such treatment regimens are able to keep the virus under control, they can also be a burden to patients. Furthermore, missing doses raise the possibility of the HIV becoming resistant to the antiretroviral drugs.
Advances in antibody technologies have opened up new avenues for research
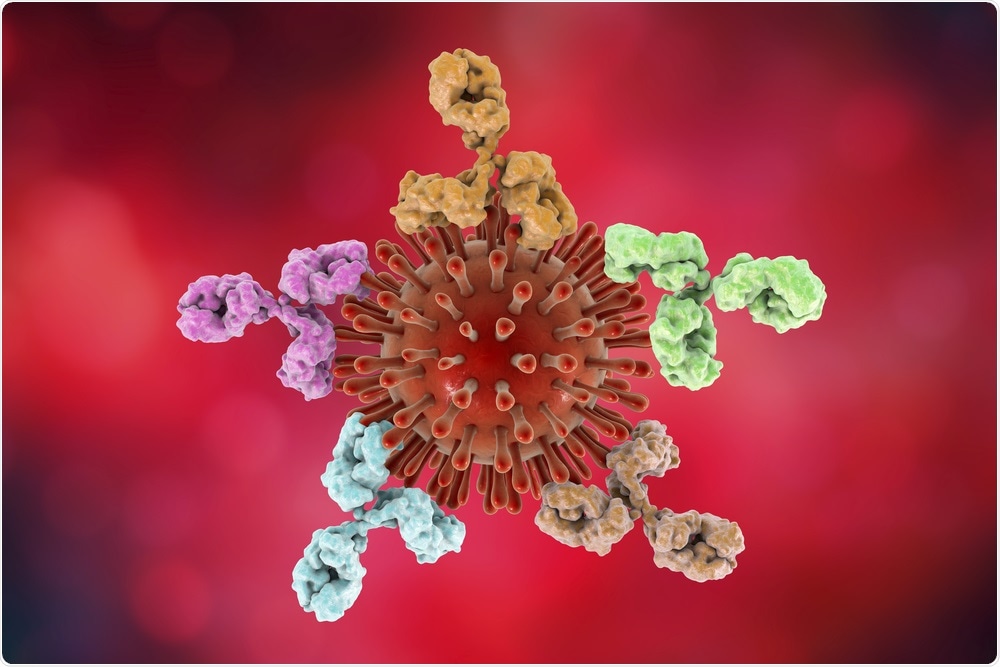
Researchers have been working on developing potent and broadly neutralizing antibodies against HIV for many years now. Such antibodies are being investigated as a potential means of preventing viral rebound after the discontinuation of antiretroviral therapy to allow patients to take a break from taking so many pills without detrimental effects on their health.
One such antibody, VRC01, was shown to slightly delay the resurgence of HIV on interruption of their usual treatment. However, it did not maintain viral suppression.
The latest clinical trial evaluated a novel antibody, known as UB-421, in patients with HIV during a short-term break in their antiretroviral regimens. On average, the patients had been taking antiretroviral drugs for over 5 years.
All of the study participants had undetectable levels of HIV in their blood and received eight injections of UB-421 (either weekly or biweekly).
HIV levels remained below the limit of detection in all patients for up to 16 weeks. UB-421 was therefore proven to effectively control HIV from replicating further and spreading infection. Furthermore, no evidence of HIV resistance to UB-421 was observed. However, due to the small size of the study, future clinical studies with long-term monitoring for drug-resistant HIV strains are needed.
‘A single agent’ to replace a ‘cocktail of drugs’
Lead author Chang-Yi Wang commented “We were able to use this antibody to maintain durable viral remission using a single agent instead of a cocktail of drugs. Such durable maintenance is unprecedented, and it opens up a host of potential new treatment options for patients with resistance-prone HIV infection.”
UB-421 acts to prevent HIV infecting immune cells by blocking the binding site. It binds to immune cells with 50 to 100 times greater affinity than HIV, and so binds in preference to the virus.
Ex-vivo studies have shown UB-421 to have a significantly greater viral inhibition capability than VRC01 and other previously tested HIV-neutralising antibodies.
This research is a promising first step towards making it possible for patients with HIV to control their infection with a weekly or biweekly treatment instead of a daily cocktail of tablets. A clinical study is now being designed to test UB-421 in people with HIV infection who have not yet start anti-retroviral therapy to see if the antibody can suppress HIV activity for up to six months.
Source:
Wang C-Y, et al. Effect of Anti-CD4 Antibody UB-421 on HIV-1 Rebound after Treatment Interruption. N Engl J Med 2019;380:1535-45. DOI: 10.1056/NEJMoa1802264.