Long-term hemodialysis is a lifesaver for approximately half a million patients in the United States with kidney failure (also known as end-stage renal disease, or ESRD) who are either waiting on or unsuitable for a kidney transplant. But before the external machinery can take over the function of the kidneys — filtering and cleansing wastes from the blood — a minor surgical procedure is needed to create a stable, functional and reusable access to the circulatory system, usually through blood vessels in the arm.
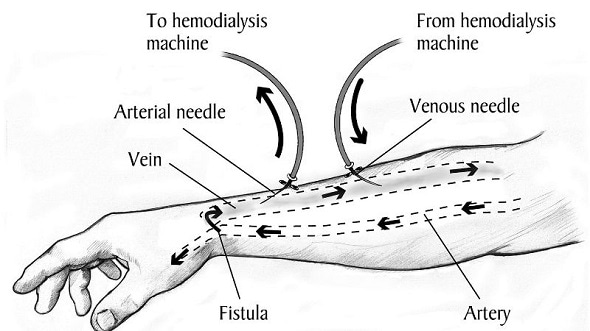
A diagram showing how kidney dialysis is conducted after an arteriovenous (AV) fistula surgery has provided access to the circulatory system. A new Johns Hopkins Medicine study reveals that many physicians are still performing a different, riskier procedure with a prosthetic graft for gaining access. Credit: National Institute of Diabetes and Digestive and Kidney Diseases/National Institutes of Health
Two surgical methods for creating this “vascular access” are available, one overwhelmingly preferred whenever possible for its better durability, performance and safety. However, in a study using Medicare claims data, Johns Hopkins Medicine researchers report that one-fifth of seasoned U.S. surgeons are statistically performing the less-preferred procedure too often, even when unnecessary, and that providing them with a peer evaluation of such performance may lead to improved practices.
The findings are reported in a new study in the current issue of the Journal of the American Medical Association Surgery.
The good news from our survey data is that progress has been made in the last decade toward reducing the number of inappropriate vascular access surgeries performed in the United States. But the numbers also show that we still have a ways to go to meet established standards that are already the norm in Europe and Asia.”
Caitlin Hicks, M.D., M.S., assistant professor of surgery at the Johns Hopkins University School of Medicine and lead author on the JAMA Surgery paper
The two types of vascular access procedures available for extended hemodialysis are the arteriovenous fistula (AVF) and the AV graft (AVG). The AVF is made by connecting a vein, most often in a patient’s arm, to a nearby artery. Over a period of two to three months, this bridge, known as a fistula, increases blood flow and pressure to the vein to enlarge and strengthen it. Once matured, the “supervein” will withstand repeated needle insertions that would collapse an untreated vessel.
In contrast, the AVG uses an artificial device, a plastic tube, to make the artery-vein connection. Because it does not require maturation, the graft can be used within three to four weeks after surgery. However, studies have shown that it is more likely than an AVF to have problems with infection and blood clots, and may need repair or replacement within a year. Additionally, according to Medicare data, the average annual cost for creating and maintaining an AVG is higher than that for an AVF — nearly $73,000 per person annually compared with $60,000.
Recognizing the distinct advantages of the fistula, the federal Centers for Medicare & Medicaid Services and ESRD treatment networks across the United States created the Fistula First Breakthrough Initiative (FFBI) in 2003 to increase the use of AVF to 50% of all vascular access surgeries performed. When that goal was reached in 2009, the AVF over AVG standard was raised to 66% in an effort to match the 60% to 90% rates in Europe and Asia.
In a bid to document progress toward that goal, and identify “physician characteristics” linked to higher-than-appropriate AVG use, Johns Hopkins Medicine researchers used Medicare fee-for-service claims data for more than 85,000 adult kidney failure patients who received first-time vascular access surgeries between Jan. 1, 2016, and Dec. 31, 2017. They calculated an AVG rate (total number of vascular access operations divided by the number of AVG surgeries) for each of the 2,397 physicians who performed 10 or more procedures — either AVF or AVG — during that time. While the median, or midpoint, rate for the whole group was 18.2% (meaning that the median rate for AVF surgeries was 81.8%), there were a significant number of outliers.
We found that 498 physicians, approximately 21% or 1 in 5, performed AVG surgeries in more than 34% of their total cases. This means that they failed to meet the 66% or higher FFBI target standard for AVF use.”
Caitlin Hicks
The study indicated that most of the physicians associated with high AVG use rates — including some who were using AVG in more than 80% of their cases — had long-established practices (a median of 35.5 years since medical school graduation), were located in a metropolitan setting and specialized in vascular surgery more than general surgery.
“Since the FFBI best practice guidelines have only been around since 2003, perhaps older physicians are simply less familiar with them and have continued ‘doing business as usual,’” Hicks says. “Or they may just be seeing more complex cases and believe that fistula access is less suitable. In either case, we believe that more education and targeted intervention using peer-to-peer evaluations that urge a change in practice may help address the problem, because that approach has worked before.”
Another Johns Hopkins Medicine study recently reported that a “Dear Colleague” performance evaluation letter successfully convinced physicians nationwide to reduce the amount of tissue they removed in a common surgical treatment for skin cancer to meet a professionally recognized benchmark of good practice.
Hicks says that the research team hopes to conduct such an intervention in a future study and document its impact on improving behavior for vascular access surgery.
The AV fistula versus graft study is part of a larger Johns Hopkins Medicine effort to develop, establish and disseminate quality measures that will capture the appropriateness of care and help reduce low-value care in favor of a more patient-centered approach.
By identifying practices that are not in the best interest of the patient and providing interventions to address them, we can help physicians who are outliers, and in turn, improve the quality of care for the hundreds of patients each one treats. Physicians, for the most part, want to do the right thing, and measures of appropriateness can help guide them.”
Martin A. Makary, M.D., M.P.H., co-author of the study, professor of surgery at the Johns Hopkins University School of Medicine and an authority on health care quality
Source:
Johns Hopkins Medicine
Journal reference:
Hicks, C.W. et al. (2019) Assessment of Use of Arteriovenous Graft vs Arteriovenous Fistula for First-time Permanent Hemodialysis Access. JAMA Surgery. doi.org/10.1001/jamasurg.2019.1736.