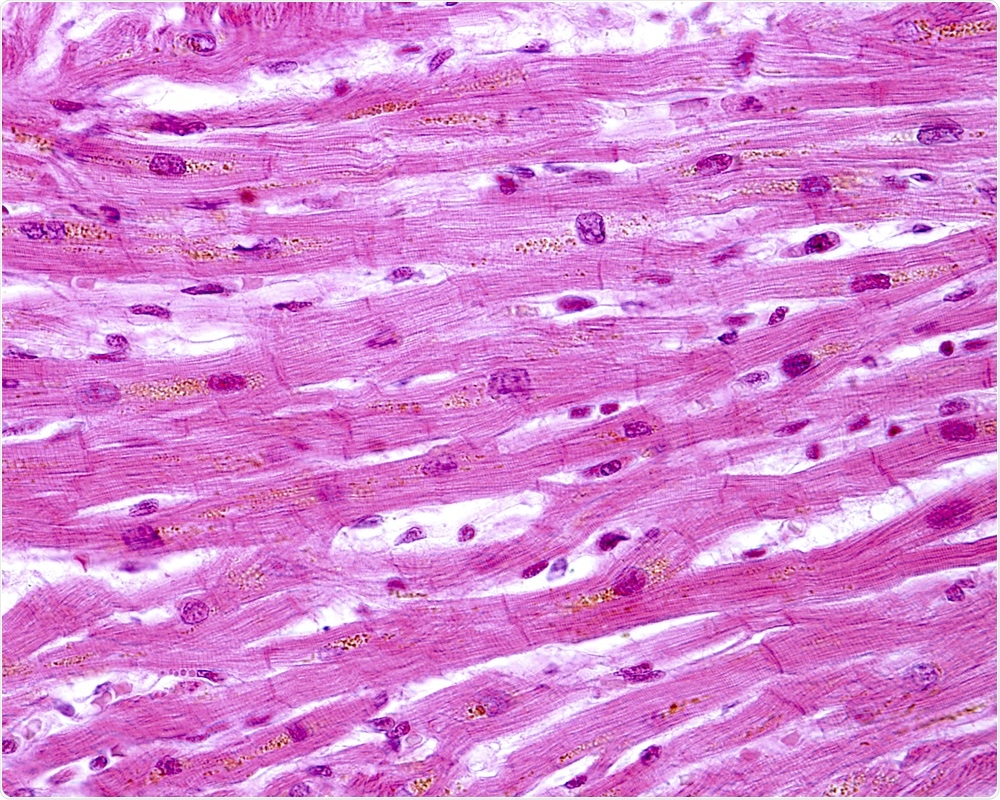
Duchenne muscular dystrophy (DMD) is a genetic, neuromuscular disease in which a patient lacks dystrophin, a structural protein present within muscle cells. This leads to inflammation and necrosis of muscles and gradual replacement of muscle tissue with fat and fibrous tissues resulting in muscle weakness.
DMD is a progressive and irreversible condition that affects every muscle group. It is more commonly seen in boys than girls and over time, leads to a decline in respiratory function. This results in patients needing clinical interventions like ventilator support, causing major morbidity and mortality. Researchers have worked on developing strategies to halt or slow down the muscle weakness to prolong lives and also improve quality of life.
Three clinical trials (named 201, 202 and 204) have been conducted on a new drug; an antisense oligonucleotide. So far, the drug has been shown to help patients with DMD. The results of the trials were published in the Journal of Neuromuscular Diseases.
 Jose Luis Calvo | Shutterstock
Jose Luis Calvo | Shutterstock
The researchers explained that respiratory function can be measured in several ways, one of which is the forced vital capacity (FVC) which is the total amount of air that can be exhaled by the lungs after a deep inspiration. This can be compared to the predicted FVC of a healthy individual of the same age to calculate the percent predicted FVC (FVC% p).
In patients with DMD who have not been treated, FVC% p starts to decline by 7 to 10 years of age. DMD usually appears by the age of 2 to 4 years. Among patients treated with steroids, the decline in respiratory functions is slightly delayed. However, the annual decline in FVC% p is around 5 percent and by the time the child reaches the second decade of his life, there is a significant decline in respiratory functions irrespective of treatment.
A decline in FVC% p to less than 80 percent causes respiratory difficulties and a value of less than 50 percent requires ventilator support at least overnight, if not during the daytime too. The researchers explain that delaying the further deterioration of respiratory function even in later years can improve the quality of life and measures to reduce this rate of decline would significantly reduce the requirement of clinical interventions in this population and improve morbidity.
Preventing respiratory decline for patients with DMD
The new drug has been approved by the FDA for the treatment of DMD. It is an “exon skipping antisense oligonucleotide” that modulates the genetics of the DMD patients to slow the progression of their disease.
This study was led by Dr. Navid Z. Khan, Senior Director, Global Medical Affairs, Sarepta Therapeutics, Inc., Cambridge, MA, USA. He and his team assessed the effect of a new drug on respiratory functions in DMD patients from three clinical trials and compared it with patients from Cooperative International Neuromuscular Research Group Duchenne Natural History Study (CINRG DNHS) global database.
Data from more than 400 DMD patients were divided into three cohorts, of which 13 percent have typical DMD mutations. These mutations can be treated by the exon 51 skipping therapy, explain the researchers.
The first cohort was the glucocorticoid-treated patients who could be treated with exon skipping (20 in number), the second cohort comprised of all glucocorticoid-treated patients (172 patients) and the third group consisted of all glucocorticoid-treated patients who had been genotyped (148 patients).
For four years each of the trials were conducted on ambulatory or mobile patients. Once they were non-ambulatory, they were again followed up for a further 2 years. The patients were aged between 7 and 16 years.
Genes are made up of introns and exons. Exons are transcribed into the final protein, whereas introns are not. This means that mutations in exons often result in disease.
Exon skipping refers to a method by which a small molecule binds to the mutated exon and prevents the cell from copying that part of the gene. This results in a truncated, but still functional dystrophin protein that no longer produces the toxic effects that lead to DMD. The new drug uses this mechanism and has been shown to slow disease progression.
The three studies
Study 201
Study 201 was a single centre study with 7 to 13 year old male patients with DMD who were treated with oral glucocorticoids.
Study 202
This was an extension of the previous study to check the efficacy and safety of the weekly injections of the drug. This study lasted four years (216 weeks)
Study 204
Study 204 looked at boys between ages 7 and 21 years who had been genotyped and had the DMD gene mutation(s) that could be treated with the new drug. Patients were instructed to stop taking glucocorticoids 24 weeks before the start of the study. They were administered weekly intravenous solutions of the drug for 96 weeks. The study extended for 2 years with periodic FVC%p.
What did the results show?
Results from 74 patients receiving the new compared with glucocorticoid in age matched CINRG DNHS DMD patients showed that there was a significant slowing of the respiratory function decline. The slowing of FVC% p was significant when compared to untreated patients. It was therefore concluded that both quality of life and disease progression could be improved through the drug.
The results in both ambulatory and non-ambulatory patients were similar. This means that the drug could be useful even for advanced disease, say the researchers. The team explains that they could evaluate the effectiveness of the respiratory muscles by evaluating upper limb muscle function. Among non-ambulatory patients, improvement in respiratory muscle function also improved the upper limbs activity.
Results showed that the annual decline in FVC% p was reduced to 2.19 percent in one study. In the other two studies the annual decline in function of respiratory muscles was 3.66 percent and 3.79 percent respectively. The researchers suggest further studies to understand the muscle function decline rates more clearly.
The researchers concluded that there was a significant slowing of the decline in respiratory functions in patients of DMD being treated with the new drug over a follow up period of two to four years.
When translated to real life scenarios, these results may reduce hospitalizations of DMD patients caused due to respiratory ailments and also reduce the requirement of respiratory interventions including ventilator support.
Journal reference:
Eteplirsen Treatment Attenuates Respiratory Decline in Ambulatory and Non-Ambulatory Patients with Duchenne Muscular Dystrophy. Journal of Neuromuscular Diseases. DOI: 10.3233/JND-180351.