Tel Aviv scientists have published their version of a vaccine against the deadly skin cancer malignant melanoma, which arises from the pigment producing cells of the skin. This is the most feared form of skin cancer, with a high tendency to metastasize to distant parts of the body, including the brain.
The new vaccine is claimed to prevent the development of the tumor in immunized mice, as well as to prolong survival very significantly in mice with primary and metastatic melanomas. Conventional immunotherapy, especially immune checkpoint therapy, has been limited in its clinical efficacy. The reasons include a poor response in the majority of treated individuals, the emergence of resistance, and unacceptably severe side effects.
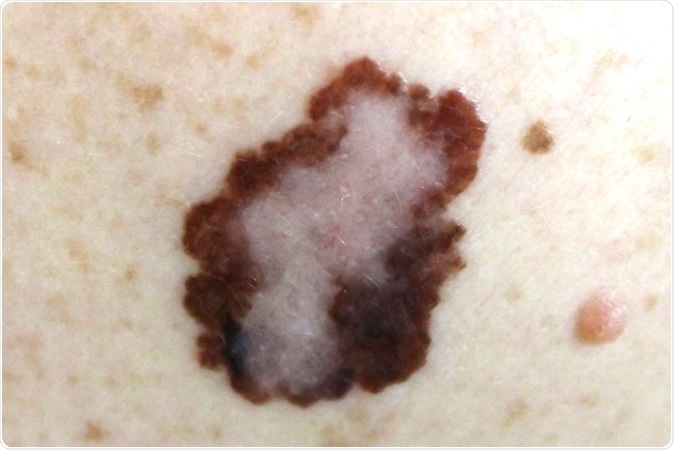
Melanoma. Image Credit: Nasekomoe / Shutterstock
In a counterattack, scientists in the Satchi-Fainaro laboratory at Tel Aviv University worked on a combination of therapies, namely, a novel nanovaccine with anti-PD-1 antibody (αPD-1). The latter works by suppressing the tumor factors which inhibited normal immune responses that would be expected to identify and attack the tumor cells as foreign, preventing tumor development and spread. They also added an anti-OX40 antibody which stimulates a class of immune cells called effector T cells. These cells respond to this molecule by proliferating and becoming more potent, surviving the effects of immune-related functions for a longer period of time.
The vaccine is composed of nanoparticles of about 170 nm size. These were built from a biodegradable polymer, and two types of peptide chains, identical to those expressed in melanoma cells, were inserted into them. These were the nanovaccines and they target dendritic cells. The combination of this vaccine with the antibodies already mentioned was then tested in a mouse model which had melanoma tumors.
Gratifyingly, the scientists found that these nanoparticles behaved very much as viral vaccines do. They stimulated the mouse immune system to recognize the malignant melanoma peptides as foreign, and this led to immune attack on all cells containing or expressing either or both of these peptides.
The researchers explored the effectiveness of the vaccine in three different situations. First, could it prevent malignant melanoma? To answer this question, they injected this into healthy mice and then implanted melanoma cells into the same mice. Researcher Satchi-Fainaro says, “The result was that the mice did not get sick, meaning that the vaccine prevented the disease.”
Secondly, mice which already had melanoma were treated with both the new nanovaccine and various forms of immunotherapy, which also boosts immunity. As a result of co-treatment with α-PD-1 antibody and anti-OX40 antibody, T-cells were found to invade the tumor in larger numbers at earlier stages. However, this did not lead to any better stoppage of tumor growth in the treated mice that already had melanomas. On the other hand, suppressor cells from the bone marrow were attracted to the tumor site, worsening the immune suppression.
At this stage, therefore, the researchers added one more drug, the monoclonal antibody ibrutinib, which targets these bone marrow-derived suppressor cells. This did the trick, stopping the melanoma cells from thriving in the immunized mice. Not only did the tumors shrink and even disappear, the mice survived for long periods of time. Thus the nanovaccine acts as an intrinsic regulator of the immune response in these sick mice, helping the body to suppress tumor growth in combination with immune checkpoint modulators. The two treatments worked together to delay the growth and spread of the malignant melanomas and gave the mice a much longer life following treatment.
As a third step, the scientists tried out the effects of the vaccine on tumor tissues extracted from patients who had melanoma metastases in the brain. The results indicate that the new vaccine can be used in the treatment of brain metastases as well. Not only so, they are looking at adapting this approach for other types of cancer as well.
Satchi-Fainaro sums it up: “Our research opens the door to a completely new approach -- the vaccine approach -- for effective treatment of melanoma, even in the most advanced stages of the disease. We believe that our platform may also be suitable for other types of cancer and that our work is a solid foundation for the development of other cancer nano-vaccines.” The new nanovaccine approach could be a beacon of hope, not only for patients with malignant melanoma, but also with other tumors which can be prevented or treated by immunizing the body against them.
Journal reference:
Immunization with mannosylated nanovaccines and inhibition of the immune-suppressing microenvironment sensitizes melanoma to immune checkpoint modulators, João Conniot, Anna Scomparin, Carina Peres, Eilam Yeini, Sabina Pozzi, Ana I. Matos, Ron Kleiner, Liane I. F. Moura, Eva Zupančič, Ana S. Viana, Hila Doron, Pedro M. P. Gois, Neta Erez, Steffen Jung, Ronit Satchi-Fainaro & Helena F. Florindo, Nature Nanotechnology (2019), https://www.nature.com/articles/s41565-019-0512-0