Stroke is the number one cause of long-term, severe disability in the US. Most often caused by a blockage within neural blood vessels either due to a clot in constricted arteries (in around 87% of stroke cases), or occasionally, caused by the opposite; a blood vessel rupture causing a leakage of blood onto the brain. Stroke is also the third most common cause of death in the US.
Those who survive a stroke often face a difficult road to recovery, with weakness or paralysis on one side of the body and marked problems with speech being common effects of this disease of the arteries.
Unfortunately, some patients do not make significant steps towards recovery due to permanent brain damage suffered as a result of the deprivation of oxygenated blood to the blood cells at the time of the stroke.
Recently, a team at the University of Calgary set out to establish what percentage of ‘low risk’ patients suffered a brain ischemia, and whether methods could potentially be put in place to predict with greater accuracy the risk of a brain ischemia in order to prevent and treat strokes with greater speed.
 Puwadol Jaturawutthicha | Shutterstock
Puwadol Jaturawutthicha | Shutterstock
Minor strokes often go undiagnosed
Fortunately, the medical sector is developing new ways to prevent stroke from occurring. It has been found that those who suffer from transient ischemic attacks (TIAs) or minor stroke have a high risk of an early recurrent stroke.
Currently patients presenting symptoms of TIA are made priority to medical professionals, however, the issue is that around half of patients do not present the classic high-risk symptoms of TIA (such as sensory symptoms). This leads these patients with transient or mild neurological deficits to not being seen as high risk for stroke.
Early detection is key to the prevention of stroke, and therefore important for reducing mortality as well as increasing quality of life after stroke.
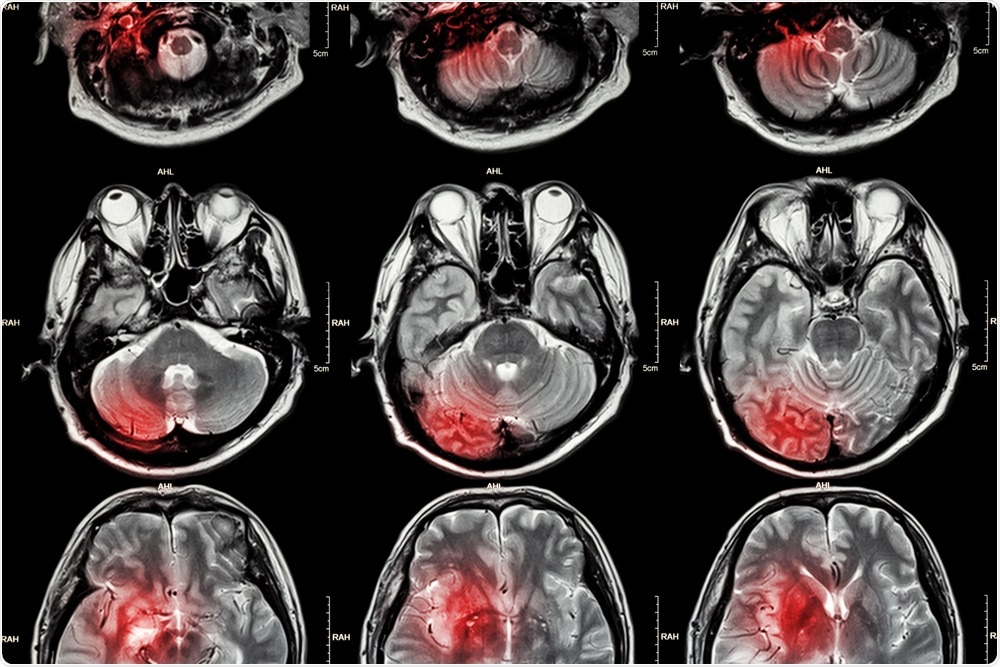
MRI in stroke diagnosis
For the past decade, MRI (Magnetic Resonance Imaging) has been considered more effective than CT (Computerized Tomography) at diagnosing stroke. Since 2010, medical professionals have been advised to favor MRI in this kind of diagnosis following new guidelines from American Academy of Neurology.
Up until this point, CT scans were the standard test for diagnosis, but it was recognized that with its ability to generate clearer images of brain tissue, MRI was more appropriate for highlighting brain regions where brain damage had occurred due to lack of blood flow resulting in restricted water diffusion through the tissue. MRI has been found to accurately detect stroke 83% of the time, compared with just 26% through CT.
MRI reveals minor stroke lower risk patients
The Canadian team, led by Dr. Shelagh Coutts, MD, used MRI to investigate 1028 patients over 6 years, who experienced nontraditional symptoms such as dizziness, numbness, or very brief periods of difficulty with speech.
The team began a study group, the Diagnosis of Uncertain-Origin Benign Transient Neurological Symptoms (DOUBT), and made neurological assessments and generated a diagnosis immediately after the onset of patients’ symptoms. Following this they conducted an MRI scan within the first week and made a second diagnosis.
The results were groundbreaking. Researchers found that these patients who had been seen as low-risk were actually at a 13% risk of having had a stroke, which was far greater than had been estimated previously.
In addition, 30% of patients had their diagnoses changed as a result of the scan. In some cases, this was because the stroke had occurred which had not been picked up previously, but in other cases, this was due to the opposite, because of a misdiagnosis of stroke in the first instance.
The results highlight the diagnostic power of MRI in stroke, as well as determining clinical risk factors for stroke. Using MRI alongside other diagnostic processes has the potential to prevent the unnecessary intake of drugs by patients misdiagnosed with stroke. It also has to potential to demonstrate where minor strokes have occurred but gone undetected.
The findings of the study also have huge implications for the clinical risk factors of stroke, showing that non-traditional symptoms are also indicative of minor stroke and that these patients should also be treated as high risk. With this knowledge, medical professionals may be able to prevent stroke and treat patients more effectively.
Journal reference:
Coutts SB, Moreau F, Asdaghi N, et al. Rate and Prognosis of Brain Ischemia in Patients With Lower-Risk Transient or Persistent Minor Neurologic Events. JAMA Neurol. (2019). doi:10.1001/jamaneurol.2019.3063