Nanotechnology has been part of the changing world today. Nanoparticles, for instance, can help make materials lighter and stronger. They have been widely used across several industries, such as computers and medical technology.
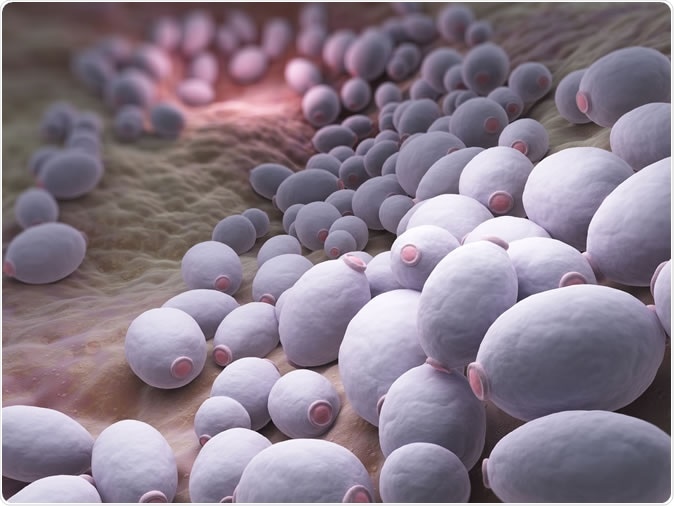
Candida albicans is a diploid fungus that grows both as yeast and filamentous cells and a causal agent of opportunistic oral and genital infections in humans - Illustration Credit: Tatiana Shepeleva / Shutterstock
Nosocomial infections are those contracted while confined in the hospital or because of medical equipment attached to the body. Invasive fungal infections are increasingly common in healthcare settings, and since the risk factors continue to rise, the infections may also soar in the coming decades. The most common nosocomial fungal causative agents include Candida species, Aspergillus spp., Fusarium spp, Mucorales, and other molds.
Candida albicans is a commonly found microorganism, but it can be life-threatening if it starts to invade medical devices like catheters that are introduced into the body. Despite being normally found in healthy individuals, the microbe can cause serious problems for those who are sick or those with immunosuppression.
Published in the American Chemical Society journal, ACS Applied Interfaces and Material, the study highlights how nanoparticles can help prevent fungal infections in patients using catheters. The microorganism, when it contaminates the catheter or another medical device, forms a biofilm and can spread into the bloodstream and, eventually, reach the vital internal organs.
“The mortality rate in some patient populations can be as high as 30 to 40 per cent, even if you treat people. When it colonizes, it's highly resistant to anti-fungal treatments," Professor Ana Traven from the Monash Biomedicine Discovery Institute (BDI), said.
The principle is, if infections are detected and treated early, there is a higher chance of becoming healthier.
"The idea is that if you can diagnose this infection early, then you can have a much bigger chance of treating it successfully with current anti-fungal drugs and stopping a full-blown systemic infection, but our current diagnostic methods are lacking. A biosensor to detect early stages of colonisation would be highly beneficial,” she added.
To land to their findings, the team investigated the effects of organosilica nanoparticles of various sizes, surface coatings, and concentrations on the viability of C. Albicans. They also studied how these nanoparticles affected and interacted with both the pathogen and immune cells in the blood. The findings show that the nanoparticles connected with fungal cells but were not toxic to them.
Moreover, the nanoparticles don’t kill the pathogen, but they can create an anti-fungal particle through the binding of these materials to a popular anti-fungal drug.
"We've identified that these nanoparticles, and by inference a number of different types of nanoparticles, can be made to be interactive with cells of interest," Dr Simon Corrie from Monash University's Department of Chemical Engineering, said.
"We can actually change the surface properties by attaching different things; thereby we can really change the interactions they have with these cells - that's quite significant,” he added.
The researchers added that the nanoparticles can be used through using nanoparticle-based technologies in infectious and contagious diseases. However, these technologies lags behind other fields.
"The other unique thing in this study is that rather than using cells grown in culture, we're also looking at how particles act in whole human blood and with neutrophils extracted from fresh human blood," Prof. Traven, said.
"We've brought together labs with expertise in infection, microbiology and immunology with a lab that has expertise in engineering, to do state-of-the-art experiments," she added.
The team concluded that the study provides a good foundation for defining the nanoparticles and how these can be designed for clinical applications about the pathogen.
“Possible future developments include designing biomaterials that could detect, prevent, or treat bloodstream C. albicans infections, which at present have very high patient mortality,” she added.
Read the full paper in ACS Applied Interfaces and Materials, titled Characterization of Key Bio–Nano Interactions between Organosilica Nanoparticles and Candida albicans.
Journal reference:
Kaserwani, V., Kelly, H., Shankar, J., Robinson, K., Kent, S., Traven, K.A, and Corrie, S. (2019). Characterization of Key Bio–Nano Interactions between Organosilica Nanoparticles and Candida albicans. ACS Applied Interfaces and Material. https://pubs.acs.org/doi/10.1021/acsami.9b10853