An Indiana hospital is in the news for all the wrong reasons. An accidental failure by one of the seven sterilization technicians working at the hospital was recently discovered. The technician failed to carry out a single step in a protocol concerning the sanitization of surgical equipment at Goshen Hospital, over a period from April 1 to September 30. This error could have led to the potential persistence of HIV, hepatitis B and hepatitis C on the tools. If so, it could have exposed over a thousand patients who had surgery during this time to the risk of these infections.
Surgical equipment is cleaned by a prescribed multistep process, of which one step was overlooked, raising the possibility that over 1,100 patients operated on with any of the equipment improperly sterilized could have been affected. However, the hospital says the usual chemical disinfection and machine sterilization steps were followed, which “include a wide margin of safety”. The only question is, were the instruments completely sterile?
Notifications have been sent to all the possibly exposed patients, and they can avail of free testing for these infections, according to hospital sources.
What is the risk?
Patients are at risk for the following infections:
Hepatitis C is caused by the hepatitis C virus, is transmitted by blood, and the most common route is via shared injection needles or other injection equipment used to inject drugs. It may have a short-lived course with spontaneous resolution, or it may become chronic, causing long-term progressive liver damage and eventually liver failure, ending in death. The symptoms of the initial infection are extremely mild, including body ache and fatigue – or they may be absent altogether.
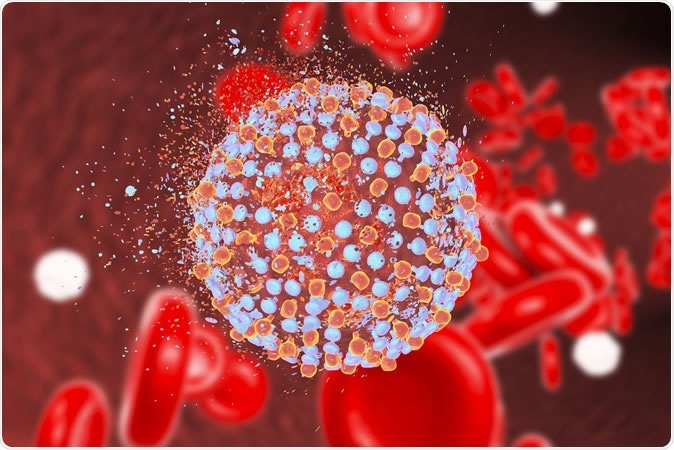
Hepatitis C virus, 3D illustration Credit: Kateryna Kon / Shutterstock
Hepatitis B is also blood-borne but is also passed through body fluids. Its course resembles that of hepatitis C.
The human immunodeficiency virus (HIV) is transferred by blood and bodily fluids as well, and causes profound depression of the immune response, weakening the body’s ability to resist infection even by very weak disease-causing organisms. If not treated with antiretroviral therapy (ART), it often progresses to full-blown AIDS, ending in a fatal termination.
The hospital’s side
According to the hospital, only a very small number of patients may have been put at risk, and the risk is “extremely low”. It also says it is offering free testing only to err on the side of caution than to take even the very low risk that any patient may be affected without knowing it. It has set up a call center to allow any patient to ask related questions or to set up a test appointment.
The hospital also says, “As with any patient safety concern, we rigorously investigated all aspects around the incident. We have put strict policies and additional safety measures in place to ensure it does not happen again.” No disciplinary action has been taken against the technician at fault, as far as can be judged from its public comments.
The hospital’s president, Randy Christophel, and chief medical officer, Dr. Daniel Nafziger, say, “While our sterile processing and infectious disease experts believe that the potential transmission of blood borne viruses between patients is extremely remote, out of an abundance of caution we want to verify through lab blood tests that patients have not been harmed.”
Patients have not been slow to react. Linda Gierek, who was operated on at the hospital on June 24, has already sued the hospital in a class-action litigation on November 22, listing several unnamed defendants at the hospital. The suit cites “negligence leading to the endangerment of lives.” Other patients are angry that they may have even potentially been exposed to an infection which threatens not just their lives but that of their families or spouses.
Low risk for transmission
Disinfectants that have been approved by the Food and Drug Administration for the high-level disinfection of surgical tools that may be damaged by heat include glutaraldehyde at a concentration of 2.4% or more, ortho-phthalaldehyde 0.55%, glutaraldehyde 0.95% with phenol/phenat 1.64%, 7.35% hydrogen peroxide with 0.23% peracetic acid, ad so on. Most of these chemicals have been tested for efficacy under worst-case conditions. These techniques assume that such contact between the equipment and the chemical will completely eliminate mycobacteria even if they are present on the most inaccessible places on the equipment and if the equipment is exposed to the agent without cleaning. This stringent standard provides for a wide margin of safety even if the processing should at any time be suboptimal, lending credence to the hospital’s assurance that the actual risk of infection is remote. As long as FDA-labeled products are used, this assurance holds good.