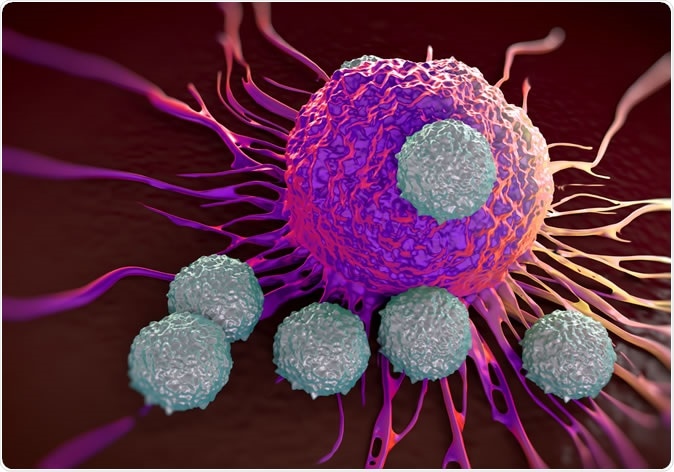
T-cells attacking cancer cells - Illustration Credit: Shutterstock
The scientists have used this new technique to quickly examine over 12,000 compounds to select those drugs that can beneficially affect exhausted T cells. They found 19 of them.
Not only can this method identify such compounds, but it can also provide a rapid analysis of the T cells to help researchers understand just how these drugs produce their effects.
T cell receptors and T cell exhaustion
The method is built on the fruits of decades of research at the laboratory of Michael Oldstone, at Scripps Research, by current and former researchers who carried out experiments in animals to understand the dynamic interaction between the lymphocytic choriomeningitis virus (LCMV). One viral strain called clone 13 is unique in being able to set up a persistent infection by producing exhaustion of the T cells that act specifically against the infection. In order to achieve this, it sends stimulatory signals via T cell receptors like PD-1 and IL-10, called inhibitory checkpoint receptors. Persistent stimulation leads to exhaustion, which is utilized by the cancer cells to survive and proliferate. This was rapidly followed by the recognition that many other cancers use the same mechanism to ensure their survival.
Among the most effective anticancer drugs today are PD-1 inhibitors and other similar inhibitory compounds that prevent signaling through these receptors, and thus help T cells regain their immune capabilities. In fact, such therapies have saved the lives of many cancer patients who would earlier have been called untreatable.
Inhibiting multiple T cell activation mechanisms
On the other hand, these drugs don’t work equally well for all cancers. Melanomas are among the most responsive, along with a few other tumors. This has led researchers to think that cancers typically inhibit T cells by more than one pathway. In that case, we should use a combination of drugs to prevent multiple methods of cancer-induced T cell failure, to achieve a better response over a greater variety of cancers. Again, the use of small molecule inhibitors may replace the blocking biologic drugs used for this purpose today.
How it works
The current study is driven by this need to develop more drugs that have potential for immunotherapy, and to tinker with them until the optimal combination is found.
The screening approach reported in the current study has been designed to speed up the process of identifying promising hits from an array of small molecule compounds with bioactivity. These hits should be molecules that will have better or synergistic activity with the injectable immunotherapeutic drugs now in use.
The technique takes as its basis exhausted T cells that have come out the worse from a battle with LCMV clone 13 and tests the new compounds on them, rather than inexperienced or naïve cells. The endpoint that the scientists look for is any sign that the compound being tested has the power to renew the immune activity of the T cell. It is thus very specific, and is almost completely automated, allowing thousands of compounds to be tested within a matter of days. Any compound which shows promise is automatically transferred to testing in mice to verify its activity.
Proving the technique
To validate their conclusions, the researchers ran the technique over a drug library containing over 12,000 compounds, all of which are under testing or have been approved as drugs by the Food and Drug Administration (FDA). These compounds are therefore suitable for repurposing. The new system quickly picked out 19 of them as hits – compounds that can effectively rejuvenate exhausted T cells in moderate doses, as seen by an increase in IFN-γ levels to normal within these cells.
The leading hit was ingenol mebutate, a plant-derived compound used as a gel under the name Picato, for the treatment of actinic keratosis which can sometimes cause skin cancer. Adapting some components of the system, the scientists examined the resurrected T cells. They found the restored activity was due to the ingenol-induced activation of protein kinase C enzymes, which are signaling enzymes that control the proliferation, differentiation, activation, survival and death of cells. These enzymes are known to respond to this molecule. These enzymes in turn reactivated the CD8+ T cells that were specific for LCMV, when they recognized the antigenic peptide. Thus, ingenol mebutate could be used in the late stages of cancer therapy, along with checkpoint inhibitors.
Benefits
This technique is performed in conditions that are similar to the immunosuppression that occurs in living tissues when the T cells are exhausted. The use of YFP as the marker of T cell effector activity gives a more accurate and inexpensive method of monitoring T cell effector activity. Small molecules are able to enter cells, spread more widely within a tumor and are less expensive to manufacture.
Conclusions
At present, researchers are continuing to explore the utility of more hits, to see if they will work as part of a combination treatment with anti-PD1 and anti-CTLA-4 compounds. The latter is a second T cell receptor that inhibits T cell activity. A combination of one of the hits with an anti-PD1 antibody is being trialled in patients currently.
The best thing about the current technique is its adaptability for screening compounds that have other types of effects on T cells, for instance, reducing T cell activity to mitigate the severity of autoimmune disease.
Journal reference:
Discovery of Small Molecules for the Reversal of T Cell Exhaustion Marro, Brett S. et al. Cell Reports, Volume 29, Issue 10, 3293 - 3302.e3, https://www.cell.com/cell-reports/fulltext/S2211-1247(19)31452-4